Antimicrobial Stewardship
Background
Antimicrobials include all medicines that are prescribed to prevent or treat infections caused by microbial pathogens, and include antibiotics (for bacteria), antivirals (for viruses), antifungals (for fungi) and antiparasitic agents (for other parasites).
Antimicrobials are amongst the most commonly prescribed drugs. Misuse or unnecessary overuse of antimicrobials has consequences for patients and the community.
First and foremost, it impacts upon the quality and safety of patient care. If a patient is not receiving the recommended best therapy to prevent or treat infection, then they have a higher risk of morbidity and mortality. Antimicrobial agents and therapies, like all medicines, carry the risk of adverse effects. These may include side effects such as nausea and diarrhoea, allergic reactions, effects of drug-drug interactions (e.g., cardiac arrhythmias) or other severe consequences such as antibiotic-induced Clostridium difficile
colitis, which in itself can lead to morbidity and death. A patient is exposed to these risks unnecessarily if they are prescribed antimicrobial treatments that they did not need.
Vision
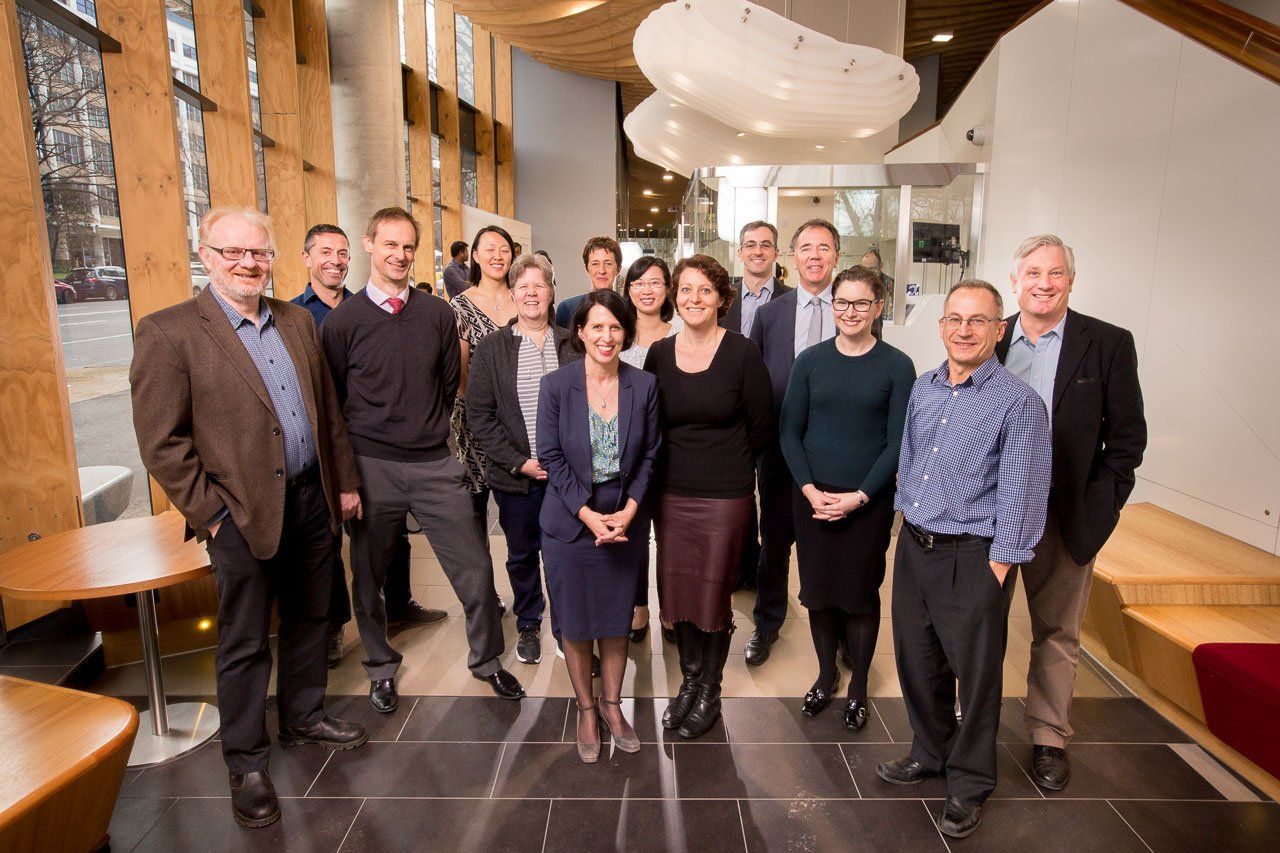
Our vision is to provide education and training in antimicrobial stewardship (AMS) and help with the implementation of AMS programs. The information on this webpage has been written by a multi-disciplinary team, some with over two decades of experience in developing, implementing and managing AMS programs in hospitals in Australia, and supporting AMS activities in the Asia-Pacific region. The modules listed on this page are intended to be used primarily by people involved in AMS programs within the hospital setting. This includes large hospitals with specialist services, small community hospitals, day procedure centres, hospitals in regional or remote areas, and hospitals funded by either the government or the private sector.
The information and resources provided here may serve to support the implementation of new AMS programs and also to generate ideas about how to improve existing programs. The authorship team acknowledges that evidence changes over time, and the ideas presented here will evolve over time. Importantly, we expect that the information outlined here will require customisation to suit local contexts. AMS must be embedded in everyday practice and thus needs to be practical in order to be accepted, utilised and sustained. There is no uniquely correct way to implement and run a hospital AMS program. Different hospitals are likely to confront different issues, and hence innovation and flexibility will always be crucial. We can all continue to learn from one another as programs are developed and refined, building a knowledge base that will help to ensure that antimicrobials are effectively preserved long into the future.
Funding support for the development of these modules was provided by the World Health Organisation Western Pacific Regional Office.
Scope
This webpage has been designed to outline the core principles of AMS that may be used in the implementation of a new or existing AMS program.
The primary objective is to provide a framework to help guide primarily acute care facilities in developing structures and governance for AMS, and outlining the education, training and resources required for an effective AMS program. This information has been written based on experience of implementing AMS in Australian hospitals. As such, it may be most relevant to hospital-based staff; however, it can be used by people in other settings. The secondary objective is to provide strategies to influence behavioural change around antimicrobial prescribing and reduce inappropriate use.
A third objective is to outline the core components of an AMS program that may be implemented as part of minimum standards for hospital accreditation. These components could be assessed by a national credentialing body, to ensure compliance with standards and allow formal registration.
Intended audience
The intended target audience includes:
- Staff of acute care facilities who are responsible for the implementation or day-to-day running of AMS programs within a facility.
- Decision-making executive or administrators of acute care facilities looking to implement an AMS program.
- National-level policy-makers responsible for the establishment and implementation of national action plans for combating AMR.
The information in these modules is intended to be used by people primarily involved in AMS in acute care hospitals. It has been designed to provide evidence-based, expert consensus on the required and recommended components of an AMS program. It aims to provide guidance to those who have initiated (or are planning to initiate) quality improvement and patient safety activities that will help manage the threat of AMR. The target audience includes staff from large hospitals with specialist services, small community hospitals, day-procedure hospitals, hospitals in rural and remote areas, and public and private hospitals. Although AMS in community settings is not the primary focus of these modules, the general principles outlined here could be used for AMS programs in the general practice, aged care, and veterinary and agricultural settings as well.