Antimicrobial Stewardship
Policy drivers for antimicrobial stewardship
In 2015, the World Health Assembly devised the Global Action Plan on AMR.
The goal of the Plan is “to ensure, for as long as possible, continuity of successful treatment and prevention of infectious diseases with effective and safe medicines that are quality-assured, used in a responsible way, and accessible to all who need them”.
To achieve this goal, the Plan sets out five strategic objectives:
- to improve awareness and understanding of antimicrobial resistance;
- to strengthen knowledge through surveillance and research;
- to reduce the incidence of infection;
- to optimise the use of antimicrobial agents; and
- to develop the economic case for sustainable investment that takes account of the needs of all countries, and increase investment in new medicines, diagnostic tools, vaccines and other interventions.
It calls for all countries to develop national action plans to address AMR. Many countries have done this.
In September 2016, the United Nations General Assembly
called upon the WHO, together with FAO and OIE, to finalise a global antimicrobial development and stewardship framework to: “support the development, control, distribution and appropriate use of new antimicrobial medicines, diagnostic tools, vaccines and other interventions, while preserving existing antimicrobial medicines, and promoting affordable access to existing and new antimicrobial medicines and diagnostic tools, taking into account the needs of all countries and in line with the Global Action Plan on Antimicrobial Resistance”.
The objective of the global antimicrobial development and stewardship framework is to support:
- research and development: support the development of new affordable antimicrobial medicines, diagnostic tools, vaccines and other interventions for detecting, preventing and controlling AMR;
- access: promote affordable access to existing and new antimicrobial medicines, vaccines and diagnostic tools of assured quality; and
- stewardship: preserve antimicrobial medicines by taking measures to promote their control, appropriate distribution as well as appropriate use.
The explicit mention of ‘stewardship’ and promotion of ‘appropriate use’ of antimicrobial medicines is critical in these documents. These are important 'top-down' drivers for the adoption of AMS practices in countries around the world.
The key challenge is promoting action at the hospital level. The ability of a government to oversee or influence the actions of an organisation depends somewhat on the organisation of the healthcare system in that country. Each country’s national action plan for AMR needs to be accompanied by a detailed plan for implementation. The plan needs to consider what policy levers are available and how specifically healthcare organisations can be motivated to take action.
In some countries, hospital accreditation can be used as a strong lever.
Hospital accreditation
According to the Australian Council on Healthcare Standards, "Accreditation is public recognition by a healthcare credentialing body of the achievement of accreditation standards by a healthcare organisation, demonstrated through an independent external peer assessment of that organisation's level of performance in relation to the standards." It should be considered separate to licensure, which is usually a government regulatory responsibility designed to set the minimum standards to protect health and safety of the public. The ministry of health is usually the licensing authority and uses this process to determine which hospitals or providers can operate or require punitive measures (if the provider is found to be substandard).
Accreditation sets standards that are considered optimal and achievable, and which aim to engender a culture of continuous quality improvement. In many countries, the accreditation process is a voluntary program that is administered separately from the ministry of health by a non-governmental organisation or by a quasi-regulatory agency. In others, accreditation is managed within the ministry of health. In most countries, the hospital accreditation program is embedded in a strong supportive governance structure by means of law and/or government policy, so that there are clearly defined frameworks for governance, scope of responsibility and authority.
The standards generally address critical elements of quality and safety in healthcare such as patient care processes, medication management and safety, infection prevention, blood products, diagnostic services, anaesthesia and surgery, patient education, and continuity of care. There will also be standards around governance, financial management, staff credentialing, human resources, building safety, patient rights and ethics, and medical record management.
There is increasing recognition that there cannot be a ‘one size fits all’ approach and that the standards should recognise difficulties encountered in under-resourced or small facilities, or in specialised institutions such as paediatric or psychiatric hospitals. Accreditation organisations aim to have surveyors who are well-trained, knowledgeable and objective, and who are able to inspire and motivate the organisation. Some countries experience serious challenges and barriers to effective review, such as corruption, remoteness and poor information management systems.
Many LMICs are undergoing significant transformation with health care reforms that aim to achieve universal health coverage. National accreditation systems have become increasingly more common and are an important strategy to improve the quality and safety of healthcare. These quality and improvement structures can be applied to the domain of AMS.
Antimicrobial stewardship accreditation
There are few countries that specifically include AMS in their hospital accreditation programs. In most cases, these standards are high-level and do not attempt to specify in great detail the requirements of an effective hospital AMS program. Many elements are already represented within standards for medication safety and infection prevention. However, any standards for AMS should attempt to outline what should be achievable within the relevant country's healthcare system.
AMS-specific standards from the Australian National Safety and Quality Healthcare Standards (2nd Edition, 2018), the Canadian Required Organisation Practice for Hospitals and Joint Commission International Accreditation Standards for Hospitals are included below.
- Australian National Safety and Quality Healthcare Standards (2nd Edition, 2018)
- Canadian Required Organisational Practices Handbook (2017)
- Joint Commission International Accreditation Standards for Hospitals (6th Edition, 2017)
In Australia, in their first iteration, the AMS accreditation standards were quite general and non-specific. They required hospitals to have an existing AMS program, and prescribers to have access to nationally endorsed prescribing guidelines. They also required some form of auditing of antimicrobial prescribing practices in hospitals, and that action was being taken to improve prescribing practices in response to audit findings. These did motivate significant activity in the area. They were introduced in 2013, and by 2015, all hospitals needed to meet these standards to be accredited for ongoing practice. In the USA, the Joint commission standards were enacted in January 2017 and required hospitals to have AMS programs in place to receive particular streams of funding.
There has been recent
publications
outlining core elements of an AMS hospital program and, within each element, a series of activities that might be achievable. This list is intended to be globally applicable and could be utilised by countries that are newly developing quality and safety standards for accreditation.
Preparing for accreditation in antimicrobial stewardship
The accreditation process will generally involve a written report detailing the activities of the AMS program (or, if no program is in place, a report on elements that are available to support oversight of antimicrobial use), as well as a face-to-face meeting with one or more surveyors. This meeting should include key members of the AMS program, and relevant managers and executives (e.g., the director of pharmacy, chief medical officer, quality manager, etc.).
Preparation for the survey should be systematic and considered. In many cases, the survey results can be used to drive business cases for more resources and funding.
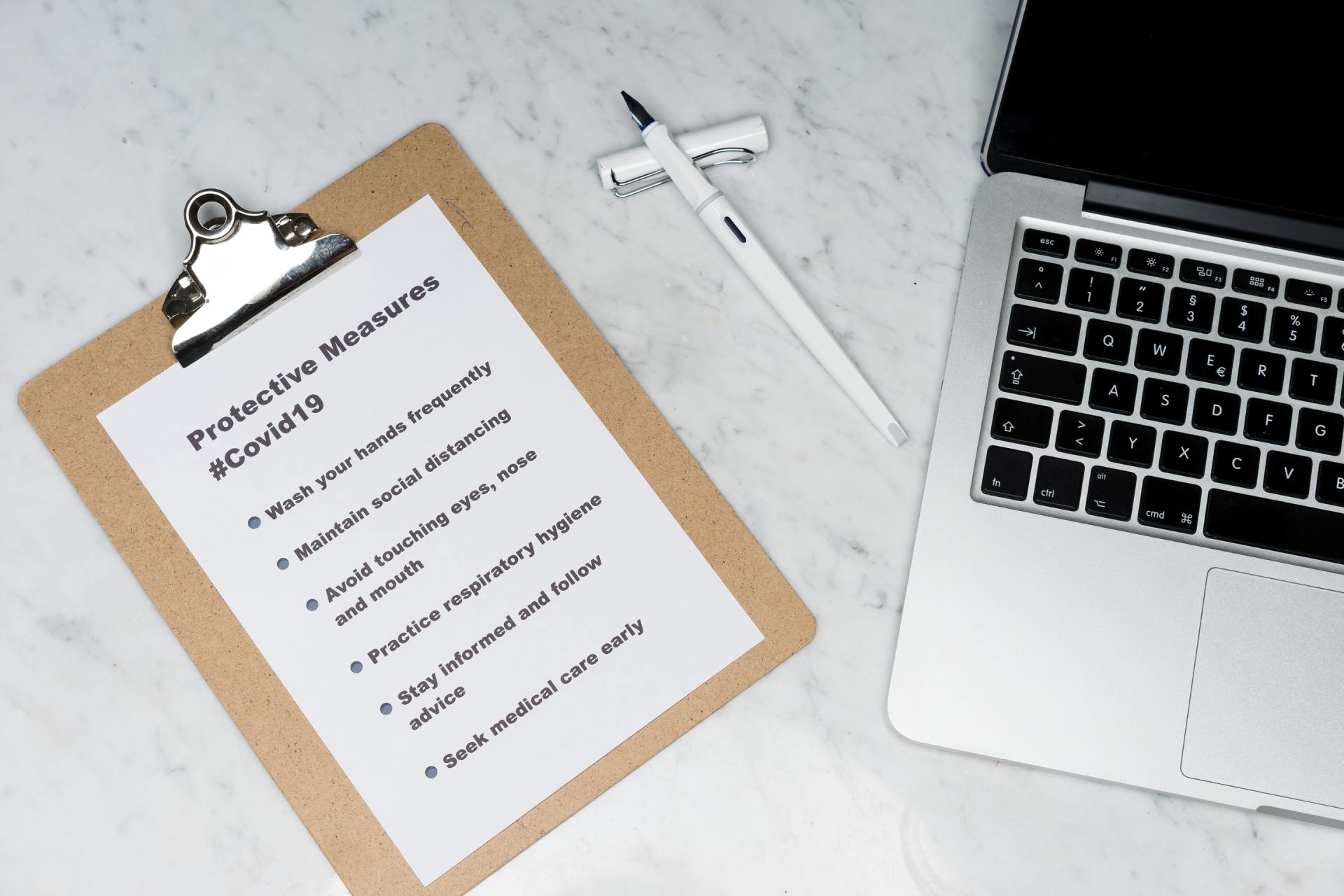
- Ensure that all members of AMS committee are familiar with the accreditation standards for AMS (if applicable), medication safety and infection prevention, as all these areas are relevant.
- Review current clinical governance arrangements and identify opportunities to strengthen or improve, e.g., hand hygiene, reprocessing reusable medical devices, workforce immunisation, AMS prescribing, and formulary restrictions and approvals.
- Identify clinical and corporate risks and identify what systems and processes are in place to mitigate those risks.
- Identify what is working well within your organisation.
- Know your risks and/or gaps – complete a gap assessment.
- Have systems to gather, review and report evidence. This might entail collating reports on antimicrobial usage and appropriateness, undertaking hospital-wide or targeted audits (e.g., surgical prophylaxis), and undertaking antimicrobial resistance surveillance.
- Have a plan to address risks and respond to the accrediting body.
- Have the ability to demonstrate progress/improvement. Aspirational goals are essential in hospitals where AMS programs are in their early phase.
- Don’t work alone; engage with others in the organisation.
Accreditation resources
An independent, not-for-profit organisation, the Joint Commission International (JCI) works to improve patient safety and quality of healthcare in the international community by offering education, publications, advisory services, and international accreditation and certification. In more than 100 countries, JCI partners with hospitals, clinics, and academic medical centres; health systems and agencies; government ministries; academia; and international advocates to promote rigorous standards of care and to provide solutions for achieving peak performance.
The Joint External Evaluation (JEE) is a voluntary, collaborative, multi-sectoral process to assess country capacity to prevent, detect and rapidly respond to public health risks occurring naturally or due to deliberate or accidental events. The purpose of the external evaluation is to assess country-specific status, progress in achieving the targets under Annex 1 of the IHR, and recommend priority actions to be taken across the 19 technical areas being evaluated. External evaluations should be regarded as an integral part of a continuous process of strengthening capacities for the implementation of the IHR.
This is an international consortium of countries implementing health financing reforms. It has published on methods to improve healthcare quality within UHC schemes, including on accreditation. It currently has 10 members from Africa and Asia. Its toolkit was created to address gaps in practical knowledge by providing guidance on setting up medical audit units, undertaking a step-by-step review of claims to identify providers prone to fraud or poor quality of care, conducting investigations, and using the results of medical audits. The medical audit toolkit is available for download from
here.
The International Society of Quality in Healthcare (ISQua) International Accreditation Program (IAP) provides a mechanism for external evaluation and standards-setting organisations to assure themselves that their standards, their surveyor training programs and they themselves, as external evaluation organisations, meet international best-practice requirements, and to demonstrate this to their clients, funders and other stakeholders.
Other resources include: