Circulars
Cellulitis and erysipelas are common bacterial skin infections, affecting the deeper layers of the skin and underlying tissues. Erysipelas is a superficial infection of the upper dermis, usually involving the facial skin but also commonly affecting the lower limbs, while cellulitis extends further into the dermis and involves subcutaneous tissue.
Both infections present as diffuse, spreading areas of skin erythema, which is often warm and tender to touch.
Cystitis is inflammation of the bladder, most commonly caused by bacterial infection and is among the most frequent infections encountered in community, hospital, and aged care settings. It is a major driver of antimicrobial prescribing and, when mismanaged, can contribute to antimicrobial resistance (AMR), adverse drug effects, and increased healthcare costs.
While cystitis falls within the broader category of urinary tract infections (UTIs), it is
typically considered an uncomplicated infection unless patient factors or clinical severity indicate otherwise. Other related conditions include catheter-associated UTIs and asymptomatic bacteriuria, while complicated UTIs include pyelonephritis and prostatitis.
Effective management of cystitis relies on accurate diagnosis, appropriate antimicrobial selection where indicated, and guidance from evidence-based guidelines or microbiology results
Read more in our latest Circular...
Oral and dental infections are generally managed with local dental interventions and addressing underlying risk factors, with the additional use of antimicrobials for limited indications. However, up to 80% of antimicrobials prescribed in this setting have been deemed unnecessary or not compliant with guidelines, for both therapeutic and prophylactic indications.
Read more in our latest Circular...
Sepsis is a life-threatening condition that arises when the body’s response to an infection damages its own tissues and organs. It can lead to shock, multi-organ failure, and death. Sepsis can often be difficult to diagnose, and is a leading cause of mortality in hospitalised patients.
Read more in our latest Circular...
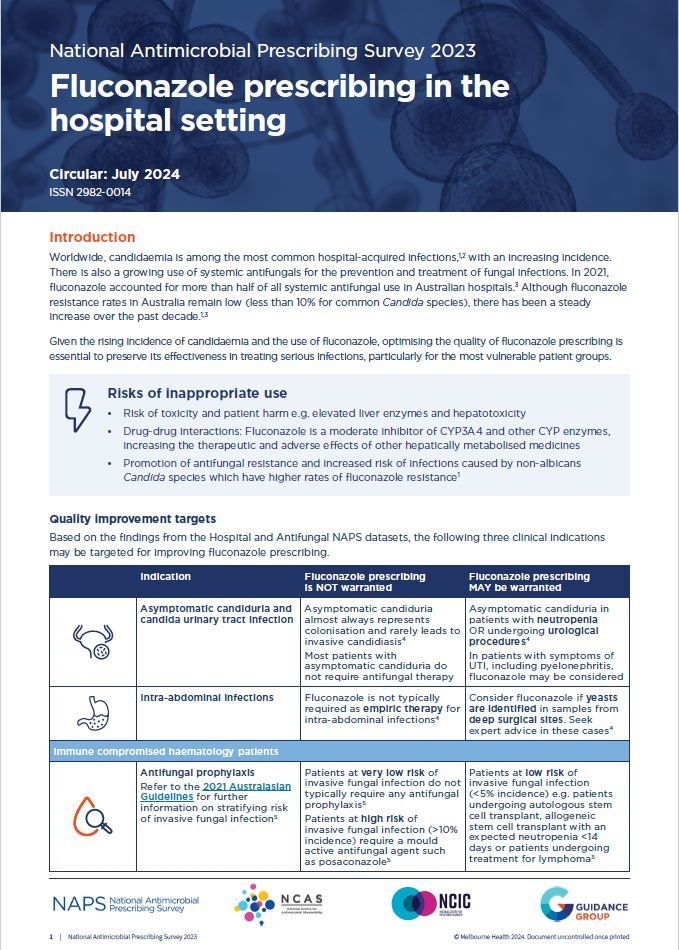
Worldwide, candidaemia is among the most common hospital-acquired infections, with an increasing incidence. There is also a growing use of systemic antifungals for the prevention and and treatment of fungal infections. Given the rising incidence of candidaemia and the use of fluconazole, optimising the quality of fluconazole prescribing is essential to preserve its effectiveness in treating serious infections, particularly for the most vulnerable patient groups.
Read more in our latest Circular...
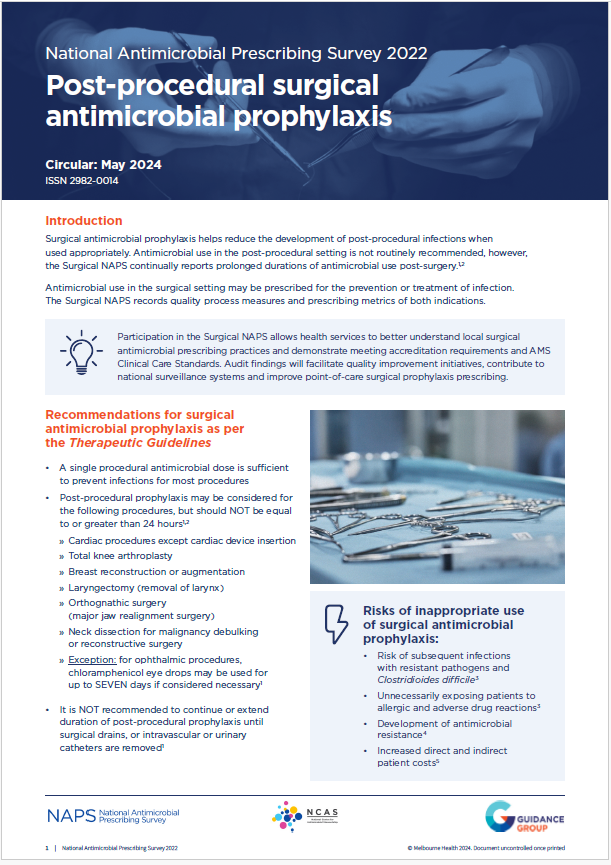
Surgical antimicrobial prophylaxis helps reduce the development of post-procedural infections when used appropriately. Antimicrobial use in the post-procedural setting is not routinely recommended, however, the Surgical NAPS continually reports prolonged durations of antimicrobial use post-surgery.
Read more in our latest Circular...
Topical antimicrobials play a crucial role in health care, by providing targeted and localised treatment and prevention for specific skin infections. They may include creams, ointments, gels and drops which are applied directly to skin, mucosa and eyes as well as surgical beads, cements, irrigations, soaks, sponges and washouts.
Data from the National Antimicrobial Prescribing Survey (NAPS) program reveals high rates of inappropriate prescribing in hospitals and high prescription volume in Residential Aged Care Facilities.
Read more in our latest Circular...
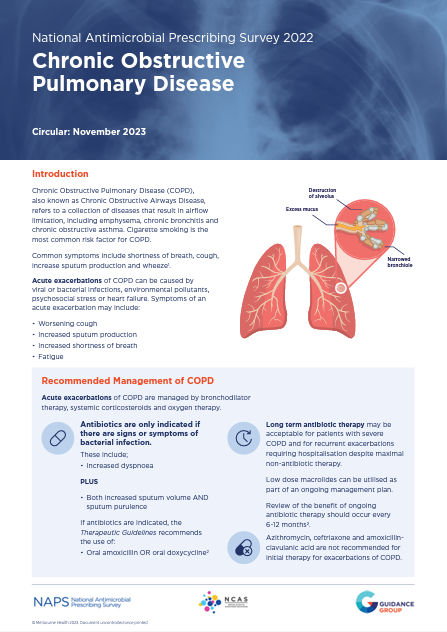
Chronic Obstructive Pulmonary Disease (COPD), also known as Chronic Obstructive Airways Disease, refers to a collection of diseases that result in airflow limitation, including emphysema, chronic bronchitis and chronic obstructive asthma. Cigarette smoking is the most common risk factor for COPD. Common symptoms include shortness of breath, cough, increase sputum production and wheeze.
COPD has consistently featured as an indication with one of the highest rates of prescribing inappropriateness and noncompliance with guidelines in the Hospital National Antimicrobial Prescribing Survey (NAPS).
Read more in our latest Circular...