Antimicrobial Stewardship
Fundamentals of antimicrobial stewardship
This module provides a framework for the modules that follow. It aims to describe how the elements required for effective implementation of hospital AMS programs relate to one another. It describes just one of many possible frameworks. This, however, is one that has served many services well in Australia and has been refined over decades as more experience has been obtained and more information from scientific studies has become available. More detail on each of the elements highlighted will then follow in subsequent pages.
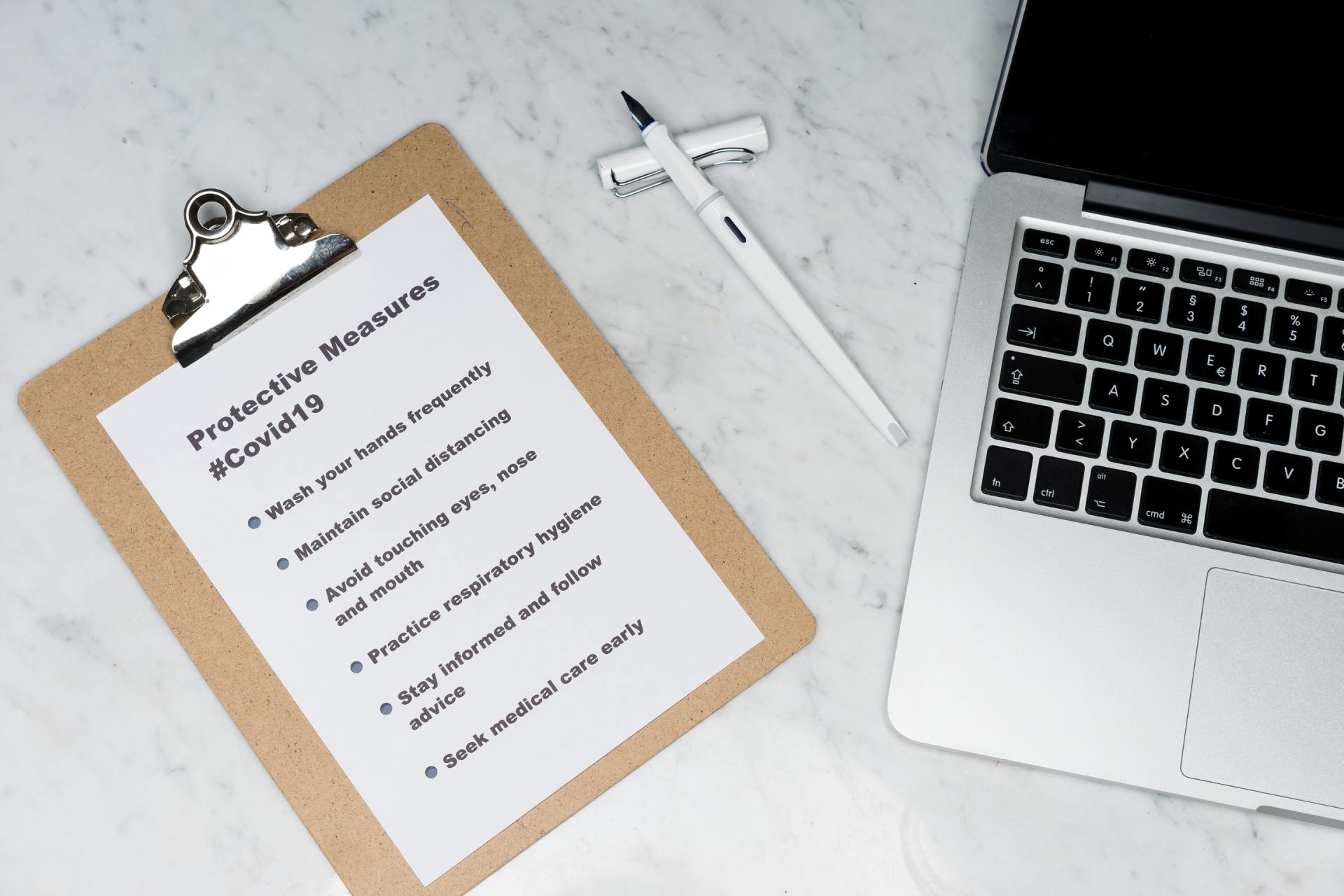
What is antimicrobial stewardship?
Antimicrobial stewardship is a term used to describe a collection of activities aiming to optimise antimicrobial therapy to improve patient outcomes (through most effective treatment and prevention of infection), while limiting the impact on local microbial ecology (limiting the emergence of antimicrobial resistance in pathogens), minimising the effects of drug toxicity for patients, and minimising cost where possible (but never at the expense of quality and safety of care).
The word ‘stewardship’ refers to the concept of ‘guiding the judicious use of a precious resource’. It could be applied to judicious-use activities for many shared resources whose long-term viability is threatened by short-term misuse.
The aim is to optimise use in situations where antimicrobials are required and reduce any unnecessary or inappropriate use. In order to do this, an organisation needs to:
Determine evidence-based best practice
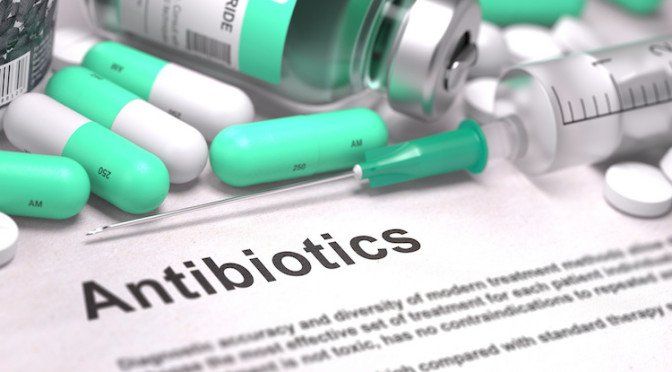
We need to be able to interpret evidence to understand what uses of antimicrobial drugs are proven to be beneficial, and in what situations antimicrobial use is simply unnecessary or potentially harmful. The key priority is to ensure, when antimicrobials are proven to lead to better outcomes for patients, that we know which the right drugs are to use, that they are available, and that we use them in the right way (correct dose and duration).
We need to understand how to limit overuse by understanding the minimum effective durations of therapy; to target drugs at pathogens promptly to avoid unnecessary broader-spectrum therapy; and to stop therapy when alternative non-infective diagnoses have been made. There are more complex questions that need to be addressed for situations where the risk-benefit equation is more questionable.
Cost-effectiveness may be an important factor to consider too. In all cases, the limitations of the evidence will need to be explored. For example, you may need to consider how well it matches your clinical context. These decisions are not easy. This is where multidisciplinary expert groups can help create guidelines, which may later require local customisation.
Describe current prescribing practice
We need to be able to collect meaningful data to understand where current practice deviates from what we might view as ideal. These data may then be used to open discussions with prescribers to try to understand why deviation is occurring. “Are the guidelines impractical? Do they fail to appreciate important clinical variations? Are there any perceptions driving poor use that need to be challenged?” Reviewing local data is often the first step towards developing a better understanding of important local AMS priorities.
Implement strategies to drive improvement
This should bring current prescribing practice closer to recommended evidence-based best practice. Ensure that the local AMS program’s priorities for action are established, the available resources and tools are assessed, and interventions are designed and implemented with ongoing support and refinement to drive change.
Use policy to drive action as necessary
Policies are important to help embed activities aimed at promoting and sustaining improvement. This may occur at a governmental level, at a hospital executive level, and/or at the level of the local committee. The importance of the issue must be made clear, and lines of responsibility and accountability need to be established. AMS cannot rely solely on the enthusiasm of individuals. It must be part of everyday expectations that we do not accept poor performance and we act to make change. Policy should be used to drive action.
The key criteria: evidence, data, action and policy
To be successful, AMS relies on the nexus of data, action and policy. Good data should inform AMS. These data include the evidence that informs the recommendations, and quality data about current local practice. The data should drive actions that are supported by good policy. The impact of action needs to be monitored through meaningful analysis of data.
To carry out AMS, an organisation requires:
- EVIDENCE-based guidelines that interpret evidence (based on data from available studies) and distill it to a form that is useful at the point of care, to help define best practice.
- DATA through ongoing monitoring of what is actually happening in practice. This should include data on antibiotic use, local infection rates, local pathogen susceptibility profiles and data on patient outcomes from management of infections.
- ACTION enabled by tools and resources. This is likely to include education, prescribing policies with restrictions, decision support, approval systems, individual patient review systems, and auditing with feedback.
- POLICIES and systems of accountability with appropriate governance to help ensure that effective AMS is being implemented.
Establishing the organisational culture
At a hospital level, it is important that the AMS program is embedded within the organisation’s broader ‘quality and safety’ framework. Indeed, an AMS program is unlikely to be successful in isolation. It is important that there is an organisation-wide commitment to a culture of promoting quality and safety. It should be clear to all staff that the hospital executive aims to ensure that patients receive evidence-based care where possible. The organisation understands that it has a responsibility to act to ensure that this is occurring.
From a practical point of view, it is likely that there will be several other activities in different sectors of quality and safety that will align with the activities of the AMS program. For example, the infection prevention program, the medication safety program, the hospital quality committee, and/or the patient safety program may all be working on similar issues. These may be able to leverage one another's activities and learn from their successes and failures, so lines of communication need to be open.
When establishing an AMS program, it is critical to ensure that it is clear to all stakeholders that the aim is to provide the best care to every person, and to deliver the most appropriate therapy to prevent and/or treat infection. AMS should be patient-centred. An AMS program should never be presented as an effort solely designed to contain AMR (e.g., being driven by the microbiology department), or as a cost-cutting exercise (e.g., being driven by the pharmacy department or the finance department). The AMS team should not be perceived to be risking poorer patient outcomes in order to limit the ecological impact or rising drug costs. The aim should be to provide good care while avoiding unnecessary harm. This requires an understanding that antibiotic overuse can cause direct patient harm. The aim of the AMS program is to use antimicrobial drugs well, to optimise outcomes and minimise toxicity, and to avoid use in situations where the risk of harm outweighs the likely benefit.
It should be appreciated that antimicrobial drugs have potential toxicity. This can include renal impairment, liver damage, vestibular damage (balance problems) or ototoxicity (hearing impairment). Correct dosing and minimising overuse should help to limit any of these adverse effects. Most prescribers readily understand this issue, and most are willing to accept expert advice to support better dosing and monitoring.
The people and their skills
Having established that patient safety is the primary driver, it is then also critical to position the AMS program as a whole-of-hospital activity. It needs to be overseen by the hospital quality and safety program, with the hospital executive being ultimately accountable for its performance. Ideally, it should be championed by clinical leaders from several different specialties. It should not be characterised as being driven by the infectious diseases unit, the microbiology unit or the pharmacy department in isolation. Surgeons, anaesthetists, physicians, nurses, infection control practitioners, microbiologists, pharmacists and others, in emergency departments, theatres, intensive care units, ambulatory care and hospital-in-the-home services, can all participate.
Staff who are tasked with implementing and managing an AMS program in hospitals need to develop a very specific skillset. Importantly, they need the ability to adopt 'systems thinking'. That is, they need to be able to think about the whole healthcare system that surrounds the pathway between a patient and their antimicrobial drug. The AMS team needs to consider all of the various stakeholders, all of the different contexts, and try to think about the many influences on the workflow of these people (taking into account what occurs in a given place at a given time). In broad terms, the AMS program is aiming to build a pathway, to guide colleagues and to make it easier for them to 'do the right thing’.
Another important skillset to develop when implementing an AMS program is 'program management' skills. In addition, managing a program over time does require creativity, energy and enthusiasm in order to find ways to sustain the messages. Program management aligns well with 'quality improvement' skills. The ‘Plan-Do-Study-Act’ cycle is one example of how quality improvement might be achieved: planning, intervening, measuring impact, and then reflecting and refining the process so that further planning is undertaken to guide further action.
Staff engaged in managing an AMS program also need to develop an ability to think in terms of population health or groups of patients, rather than individual patients. People with experience in public health can do this well, but many other hospital clinicians may never have been challenged to think in this way. Avoiding use of post-operative antibiotics for one patient for an elective procedure may seem like a low-impact intervention, but when multiplied by the number of patients presenting for elective surgery across many institutions it can impact on large numbers of patients.
Antimicrobial prescribing is a behaviour that prescribers undertake as part of everyday work activity. AMS programs strive to change this behaviour and encourage prescribers to adopt new practices. Thus, AMS requires behaviour change, and there is a theoretical framework for understanding behaviour change that can be readily adapted to help guide AMS.