Antimicrobial Stewardship
Education
Key points
- Education is a key component of any AMS program and underpins the goal of achieving sustainable changes in clinical practice at your institution.
- All healthcare professionals who have contact with patients undergoing antimicrobial treatment should receive AMS education.
- Attention should be directed towards maintaining your own personal education, providing AMS education to other clinicians and ensuring that patients receive education about their antimicrobial treatment.
- Communication skills training is an effective method of improving the way in which staff raise concerns with one another.
Education program aims
- Improve the knowledge of healthcare professionals regarding the use of antimicrobials and AMS principles.
- Change the attitudes of clinicians by persuading them that AMS strategies are effective, beneficial and easy to incorporate into the daily workflow (sustainable).
- Complement antimicrobial restriction with approval systems.
Program delivery methods
Education can be delivered in different formats, either passive or active, and using a variety of strategies and approaches to meet staff needs.
- Undertake self-directed learning, preferably with an assessment component. For example, reading journal articles or guidelines, or completing an accredited online course.
- Update your knowledge and share this information with others to influence their practice.
- Join ID-focussed professional organisations.
- Attend presentations, conferences, seminars and workshops.
- Participate in journal clubs, or access online journal clubs (e.g., our monthly webinars).
- Organise small group- and case-based discussions with a mentor who has ID expertise, or undertake academic detailing (educational visiting).
- Attend ID-related medical teaching rounds, or morbidity and mortality case reviews.
- Use these forums to learn from others, discuss ideas and share resources. They can also be used to present the results of AMS audits, projects or research and provide an opportunity to seek feedback from your audience.
- Access and disseminate information brochures or handouts.
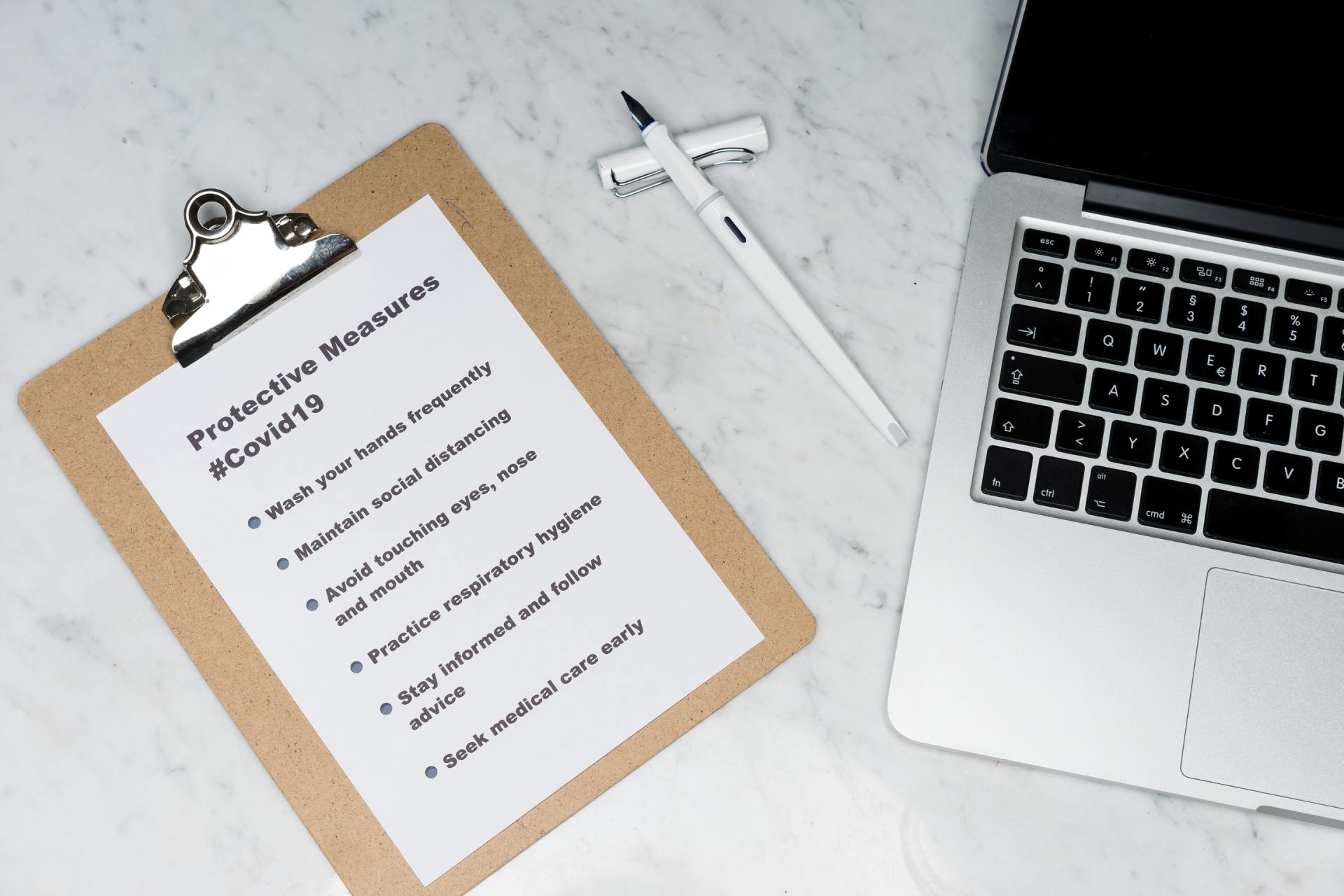
- Access and disseminate posters.
- Use lanyard cards.
- Visual material can promote specific AMS messages and educate patients, carers and staff members. Keep the content simple and easy to understand. Place posters in ward areas where staff will see them, and in patient waiting rooms. Lanyard cards with essential prescribing or guideline information can be distributed to staff.
Personal educational targets
AMS providers who are responsible for performing AMS audits and interventions, training other staff and providing support should establish competency in the following areas:
Nurses and pharmacists
Clinical knowledge and skills:
1) Pharmacology of anti-infective agents including:
- Spectrum of activity
- Clinical indications
- Principles of pharmacokinetics and pharmacodynamics (PK/PD)
- Therapeutic drug monitoring
- Common adverse effects, as well as those that are rare but significant
- Important drug interactions
2) Basic microbiology and infectious diseases:
- Diagnostic criteria, treatment options and existing clinical guidelines for common infections
- Basic mechanisms of antimicrobial resistance, common resistance profiles with corresponding risk factors, and directed treatment options
- Correct specimen collection techniques
- Limitations of current diagnostic techniques for infectious diseases
- Interpretation of microbiology results and antibiograms, their utility and limitations
3) Basic clinical skills:
- Communication with patients and healthcare providers
- Clinical review and patient evaluation, including severity of infection and patient factors affecting treatment choice
- Clinical documentation and reporting
Knowledge and skills necessary for participating in an AMS program:
1) Principles of AMS, including aims, ethical considerations and controversies
2) Quality improvement strategies
3) Project management skills
Measurements of the outcomes and impact of an AMS program:
1) Importance monitoring and feedback to drive the program
2) Process measures and outcome indicators
3) Surveillance of AMR and AMU
Doctors
AMS or ID trained physicians should have a comprehensive knowledge of all of the above competencies, as well as:
1) Comprehensive understanding of antimicrobial pharmacology and treatment guidelines
2) Comprehensive understanding of the diagnostic role of the microbiology laboratory and the principles of microbiology
3) Comprehensive understanding of infectious diseases, including diagnostic tests and their interpretation, and treatment guidelines
4) Advanced clinical skills, particularly in patient evaluation and the treatment of significant infections
Tools and resources
Beginners
1) Australian Commission on Safety and Quality in Health Care (Australia)
Think global, act local!: These video presentations describe the aetiology of AMR and the role of AMS in the hospital setting.
2) Australian Commission on Safety and Quality in Health Care (Australia)
Principles of antibiotic therapy: This video presentation describes the basic principles of antibiotic pharmacotherapy and outlines commonly seen classes of antimicrobials.
3) University of Dundee (Scotland)
Antibiotic stewardship: Managing antibiotic resistance: This free course is held approximately 3 times per year. It requires a time commitment of 3 hours per week and is conducted over a 6-week period. The course content is delivered via a mixture of lectures, articles and online discussion groups. While the course overall is more appropriate for staff with an intermediate level of AMS knowledge, the content of Week 1 would be appropriate for beginners as it covers the basics of antimicrobial resistance, the impact of resistance and how resistance develops.
4) Stanford University, Stanford Centre for Continuing Medical Education (United States)
Antimicrobial stewardship: Optimisation of antibiotic practices: This course is delivered through video lectures and Module 1 is appropriate for a beginner audience. The content includes:
- Principles of antimicrobial use
- Antibacterial pharmacokinetics and pharmacodynamics
- Sepsis case study
- Introduction to antimicrobial resistance
- Antibiotic allergies
- Management of urinary tract infections
- Management of upper respiratory tract infections
- Management of community acquired pneumonia in the outpatient setting
Intermediate
1) University of Dundee (Scotland)
Antibiotic stewardship: Managing antibiotic resistance: This free course is held approximately 3 times per year. It requires a time commitment of 3 hours per week and is conducted over a 6-week period. The course content is delivered via a mixture of lectures, articles and online discussion groups. The general course themes and content include:
- Starting an AMS service in a hospital
- Measurement – the importance of measuring antibiotic use, how and what to measure and how to measure the quality of antibiotic use
- The role of diagnostics – why diagnosis is important, how conventional and novel diagnostics can coexist, the role of biomarkers, the role of electronic clinical decision support systems, and the pharmacokinetics and pharmacodynamics of antimicrobials
- Behaviour change – behaviour change techniques and the important role of culture and team dynamics in AMS
- The final section of the course is focused on real-life examples from hospitals in South Africa, India and Scotland about some AMS interventions that they implemented and how they were able to achieve ‘quick wins’.
2) Stanford University, Stanford Centre for Continuing Medical Education (United States)
Antimicrobial Stewardship: Optimisation of antibiotic practices: This course is delivered through video lectures and Module 2 is appropriate for an intermediate audience. The content includes:
- Measurement and metrics
- The role of clinical decision support systems
- Management in specific settings such as surgical antimicrobial prophylaxis, outpatient antimicrobial therapy, paediatrics, transplantation and long-term care
Outcome measurements
- Maintain demonstrated core competencies and professional registration relevant to your occupation
- Achieve CPD targets by successfully completing recognised training courses or education programs and apply this knowledge in practice
- Stay up-to-date with the latest relevant developments in microbiology, infectious diseases management and prevention, pharmacotherapy and AMS practice
Communication skills training
Many junior doctors, pharmacists or nurses may not have the confidence to query a decision made by a senior doctor, and yet this could place a patient at risk of harm. Communication skills training is an effective method of improving the way in which staff raise concerns with one another. It forms part of general safety training in many organisations, and involves teaching staff the skills to speak up in a way that does not threaten or challenge their colleagues, but is instead received as helpful.
In a busy workplace, requests that are posed clearly and succinctly are likely to be well received. ISBAR is a widely employed technique to convey concerns in a structured manner:
- Identify – I am the nurse looking after Patient X.
- Situation – He is the man on ward 2 West admitted with pneumonia.
- Background – He was started on IV benzylpenicillin on Monday.
- Assessment – He is much improved and meets the criteria for an oral switch.
- Request – Can we switch him to oral amoxicillin instead of re-siting his IV cannula?
- “Can I just check that dose with you?”
- “The guidelines suggest we should use X grams rather than Y grams in people with renal impairment. Could we review that dose please?”
- “I would like to check that dose with the consultant before I give it because it looks like a very high dose to me and I am concerned about his renal function.”
Staff education
AMS providers are responsible for the hospital-wide education of all relevant staff. A clear educational strategy should be in place which outlines a best-practice model of patient care. Regular staff training is required to keep pace with changes in AMS practices and staff turnover.
Developing an educational strategy
1) Audience: All clinicians should receive AMS education at all stages of their training and career: doctors, nurses, pharmacists, microbiologists and laboratory staff. Ideally, training will commence early in the undergraduate curriculum. Tailor the content of the educational material to the audience’s existing level of knowledge and experience (student, junior, senior, specialist, etc.).
2) Educational calendar: Create a calendar of events, taking into consideration:
- How frequently training will need to be repeated, such as when new staff join the hospital or rotate to new areas
- Whether additional training will be required to coincide with specific events, for example, when the results of audit activities are released, or to coincide with World Antibiotic Awareness Week
- Whether there are existing events (staff orientation days, specialist unit meetings) where the AMS team could present an education and feedback session
3) Content: Consider options for content delivery:
- Face-to-face presentations
- Webinars
- Online or paper-based training modules.
Where possible, staff training should include an element of competency assessment.
Topics could include:
- The hospital AMS policy (including antimicrobial restriction and approval systems) and the principles of good prescribing
- General principles of antimicrobial therapy - how antimicrobials should be used prudently to treat common infections and the role of the healthcare professional
- The threat, causes and adverse impact of AMR, and the importance and benefits of AMS
- Diagnostic treatment guidelines and pathways
- Misconceptions about antibiotic allergies
- The concept of an antibiotic ‘time-out’ and how to utilise this strategy in practice
- Creation and interpretation of antibiotic susceptibility reports and hospital antibiograms
- Roles and responsibilities of healthcare professionals to ensure appropriate use of antimicrobials and combat AMR
- Therapeutic drug monitoring
4) Resources: Identify the resources required to run and coordinate the educational program:
- Facilitator/educator
- Venue and IT support
- A presentation and associated handouts or a take-home pack
- Feedback form or survey
5) Documentation and program assessment:
- Maintain a register of attendance. Basic training should be compulsory for all relevant hospital personnel.
- Assess whether existing educational activities or strategies are working.
- Consider what barriers have been successfully overcome and those that still remain.
- Ask colleagues for constructive feedback about both the content and delivery of the presentation or information, with the aim of improving the course content over time.
Tools and resources
1) Stanford University, Stanford Centre for Continuing Medical Education (United States)
Optimising antimicrobial therapy with timeouts: This course consists of video lectures and describes:
- The concept of an antibiotic ‘time-out’ and some general principles
- Practical ways to apply this in different settings, including pneumonia, urinary tract infections, cellulitis, ventilator associated pneumonia and febrile neutropenia
2) Wake Forest School of Medicine (United States)
An antibiotic stewardship curriculum for medical students: This course is part of the curriculum for medical students and is delivered in 3 lectures:
- AMR and its relationship to antibiotic use
- An introduction to prudent antibiotic use
- Evaluation and management of common respiratory tract infections
The small group case scenarios are intended for students to discuss (with a facilitator) how they would manage various different clinical scenarios.
3) Centres for Diseases Control and Prevention (United States)
Core elements of hospital antibiotic stewardship programs: These documents describe the 7 core elements of hospital AMS programs, accompanied by a useful checklist, and suggest some activities relating to each of these.
4) Centres for Diseases Control and Prevention (United States)
Assessment tools for antibiotic use: These forms comprise a series of questions that should be asked for each patient prescribed an antibiotic, and may be useful for AMS services to detect specific deficiencies in the prescribing for certain conditions. The forms cover 4 areas:
- Assessment of appropriateness of antibiotics for urinary tract infections
- Assessment of appropriateness of antibiotics for community-acquired pneumonia
- Assessment of appropriateness of antibiotic use for resistant Gram-positive infections
- Assessment of appropriateness of inpatient antibiotics
5) National Quality Forum (United States)
National Quality Partners playbook: Antibiotic stewardship in acute care: This document is based on the CDC Core Elements document and suggests some practical examples of activities that hospitals can conduct to support each of the CDC’s 7 core elements. The implementation examples are divided into three levels (basic, intermediate and advanced), and there are also sections on potential barriers and suggested tools and resources.
Outcome measurements
- Records demonstrate >90% attendance at compulsory AMS training and education sessions for all relevant hospital staff. Absentees are followed-up to ensure they complete their training.
- AMS audits show sustained improvements in areas that have been the target of educational campaigns, practice-change and quality improvement initiatives.
Patient-centred education
When reviewing patient antimicrobial treatment during AMS clinical rounds, take the opportunity to discuss the case and your recommendations with the treating doctor and nurse. This approach will educate ward staff and help to build relationships with clinicians in the hospital. Recommendations should also be documented in the clinical record.
Tools and resources
During AMS rounds, it will be useful if members of the AMS team can demonstrate how hospital staff can:
- Access hospital-endorsed prescribing guidelines via smartphone apps or the internet
- Use the hospital restricted-antimicrobial approval system
It can also be useful to share and distribute hard-copy resources with staff to reinforce key information:
- Lanyard cards or paper copies of antimicrobial prescribing guidelines
- Posters to display in the ward
- Information about current AMS initiatives
Outcome measurements
Patient-specific recommendations made during AMS clinical rounds have a high acceptance rate, as demonstrated in post-prescription review and audit results.
Consumer education
Patients and their carers should understand the basic principles of antimicrobial use. All consumers should understand the purpose of their medication and the treatment plan also needs to be clear, including:
- How to administer their medications
- The benefits and potential side effects of the treatment
- Where to obtain further medication supply
- How to safely dispose of any unused medications
The Clinical Care Standards in Antimicrobial Stewardship are an excellent example of what should be expected from a prescriber from the perspective of a consumer who is about to be prescribed an antimicrobial. It describes what a safe and high-quality prescription and care should include: that consumers receive adequate information, that their prescription is in line with endorsed evidence-based recommendations where possible, that appropriate tests are taken and results are acted upon in a timely way, and that any life-threatening infections are managed promptly and effectively.
Tools and resources
- Face-to-face education
- Patient-centred brochures
- Consumer medicine information leaflets
- Personalised medication lists with instructions
Examples of patient education materials
1) Australian Commission for Safety and Quality in Healthcare
2) New South Wales Clinical Excellence Commission
3) World Health Organisation
Outcome measurements
Patients and carers understand the treatment plan and can use medications safely and responsibly. Where possible, this is demonstrated in formal feedback or customer-satisfaction surveys.
Resources specific to Antibiotic Awareness Week
World Antibiotic Awareness Week occurs in November each year and provides a good opportunity for AMS programs to highlight the importance of AMR and AMS.
1) World Health Organisation: This website contains a number of campaign materials, including posters, infographics and a campaign toolkit.
2) New South Wales Clinical Excellence Commission
(Australia): This website contains tools to support some activities that hospitals can conduct during antibiotic awareness week, including a photo campaign to engage the hospital workforce, and educational talk for nursing staff and an information sheet for patients and carers.
3) Australian Commission on Safety and Quality in Health Care
(Australia): This website includes some ideas for activities that hospitals can implement and examples of presentations that AMS clinicians can present to the wider hospital audience to educate them on the importance of AMS.
4) Other international websites: