Antimicrobial Stewardship
Pre-prescription review
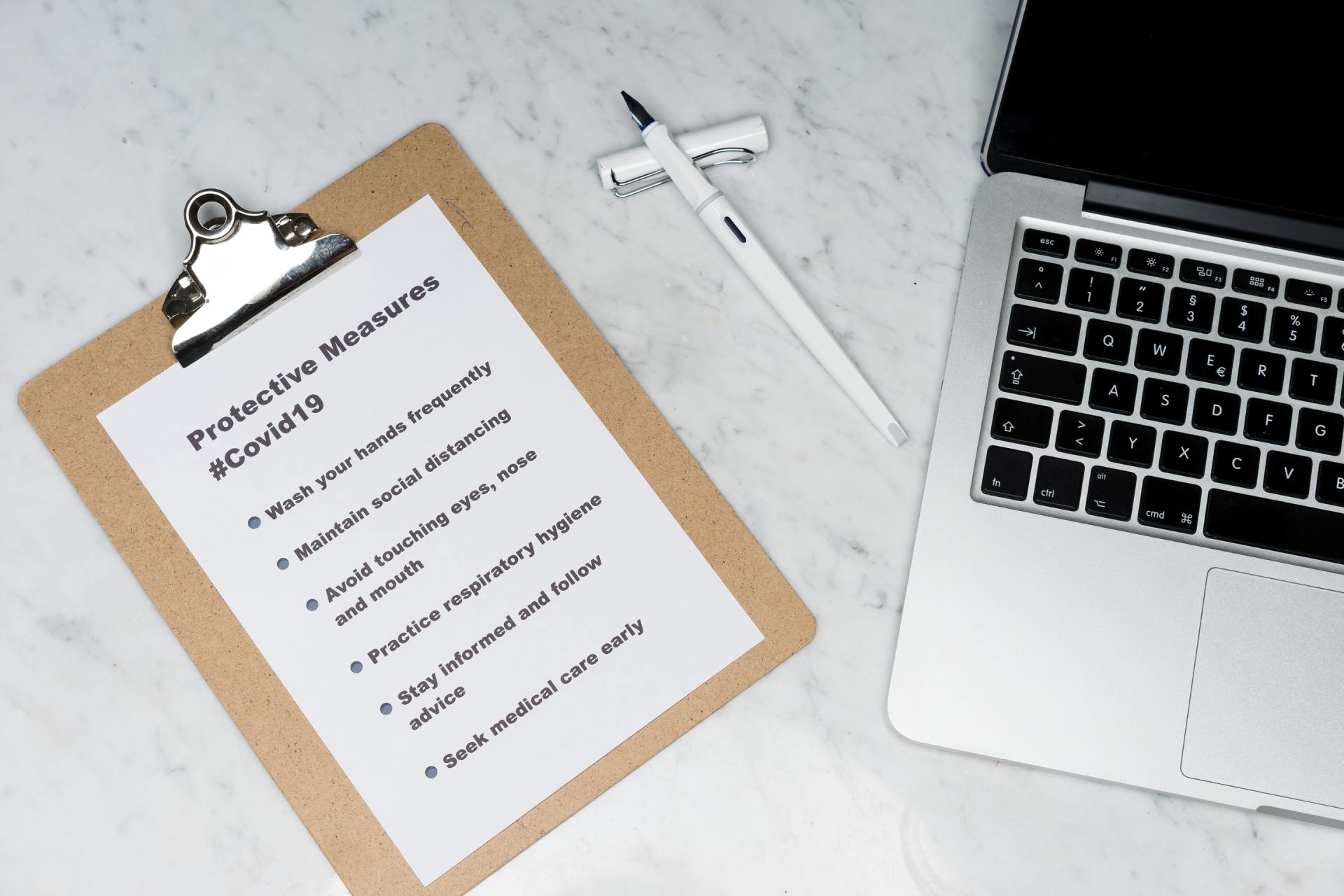
Key points
- A pre-prescription approval system is a highly effective way to rapidly change prescribing practices within a hospital.
- Pre-prescription approval involves the prescriber checking that the drug use is concordant with recommendations before administering the drug.
- Telephone approval is an inexpensive and quick-to-establish system, as it utilises existing methods of communication between prescribers and specialty groups.
- Drug order forms allow a clear record of why the drug was requested and the reasoning around approval or rejection of this request.
- Electronic approval systems are a possible solution for challenges relating to the resources involved with telephone and paper approval systems and the time taken to provide approvals in urgent setting.
A pre-prescription approval system is a highly effective way to rapidly change prescribing practices. First and foremost, it should be guided by the antimicrobial prescribing policy, and the formulary and restriction policy of the hospital. The policy needs to be accompanied by a procedure that describes how a prescriber should obtain approval.
Pre-prescription approval involves requiring the prescriber to check that the drug use is concordant with recommendations before administering the drug. This may occur via written or electronic nomination of the indication from an approved list of indications for use, or it might require the prescriber to contact a designated member of staff to gain an approval. This staff member may be an expert or part of a team including:
- infectious diseases clinicians;
- clinical microbiologists;
- physicians with an interest in antimicrobial stewardship;
- members of the DTC or similar; and
- members of the executive with oversight of medication safety, quality, or similar.
The approval is usually in the form a code made up of numbers and letters, which may be manually or electronically generated. Approval codes should be required to be documented on the patient’s medical chart or notes. If electronic prescribing is available, it may be documented alongside the medication order.
There should be explicit rules regarding whether a restricted antimicrobial can be dispensed or administered before the approval has been obtained.
In many centres, first doses of restricted drugs might be permitted with a requirement for approval before the second dose. In some centres, patients with sepsis (those on sepsis pathways) or seen during medical emergency team calls are exempt. Some centres choose to exclude the emergency department or intensive care unit from the approval requirement. In our experience, however, these can be the most valuable places to implement the system, and, with local staff engagement, the approval system can work very well in these settings.
An approval system should ideally help the prescriber. At the time of ordering, they are checking that the indication is an evidence-based acceptable indication for using that drug. If possible, additional information should be made available, e.g., doses recommended, additional drugs often used for that indication, etc., which makes the interaction valuable to the prescriber.
In all situations, it should be acknowledged that patients are highly variable and that many clinical indications for use will arise that do not neatly fit a list of pre-approved evidence-based recommendations. The system needs to have a strategy to manage this. In most cases, a pathway for obtaining approval is needed in which clinical justification can be provided by the prescriber. Often these cases will be triaged for early post-prescription review and follow up
Methods of pre-prescription approval management may include:
- telephoning an expert for approval;
- filing out a drug order form and faxing it; and
- using an electronic decision support and approval systems.
This is commonly used by many facilities as this is an inexpensive and quick-to-establish system, and as it utilises existing methods of communication between prescribers and specialty groups. It does have limitations, including for prescribers, as they have to stop their workflow to make a phone call, and for the expert who may be repeatedly interrupted from their usual work to answer multiple phone calls throughout the day. There needs to be requirements for gaining access to approvals after hours or for restricted antimicrobials to be prescribed out of hours for short durations with follow up within an acceptable timeframe. There may be inconsistencies in the advice given if the service is shared among multiple expert staff, and it is often difficult to maintain adequate records of discussions and to communicate these back to relevant staff in a timely manner.
These forms must be completed and forwarded on to the relevant specialty group or staff member for review and approval. The benefit of this system is that there is a clear record of why the drug was requested and the reasoning around approval or rejection of this request. A limitation of this system is that it is very onerous on both parties to have to complete this paperwork every time a restricted antimicrobial is prescribed. There is the risk this will slow down the time to actually administer the antimicrobial to the patient and may impact on patient outcomes if this is delayed too long, especially for sepsis. There also needs to be requirements for gaining access to approvals after hours.
Electronic approval systems are programs that allow the prescriber to gain an approval through answering a few questions to determine if the prescription is appropriate or inappropriate. Automation through the use of an electronic approval system is a possible solution to challenges relating to the resources involved in telephone and paper approval systems, and the time it takes to provide approvals in an urgent setting. They can be accessed out of hours and give an immediate response to prevent delays in obtaining an approval. They are also able to give consistent advice that has been decided and pre-determined by the AMS team or DTC. They may also be used to educate prescribers by allowing the guidelines to be visible at the time of prescribing and to alert prescribers when the antimicrobial choice is non-compliant with the recommended guideline. At the same time, they can advise on recommended dosage and duration of therapy. Their limitations are that they are expensive to implement, require easy access to computers and, therefore, may not fit the workflow of the prescribers, and require constant updating of the content to generate appropriate approvals.
In many settings, the electronic approval system may be used for the high-volume restricted drugs, e.g., the ‘amber’ drugs, while a phone approval may be required for highly restricted, less commonly used agents, e.g., the ‘red’ drugs. The approval list can help to identify patients who may need follow up through a post-prescription review system.