Antimicrobial Stewardship
Getting started
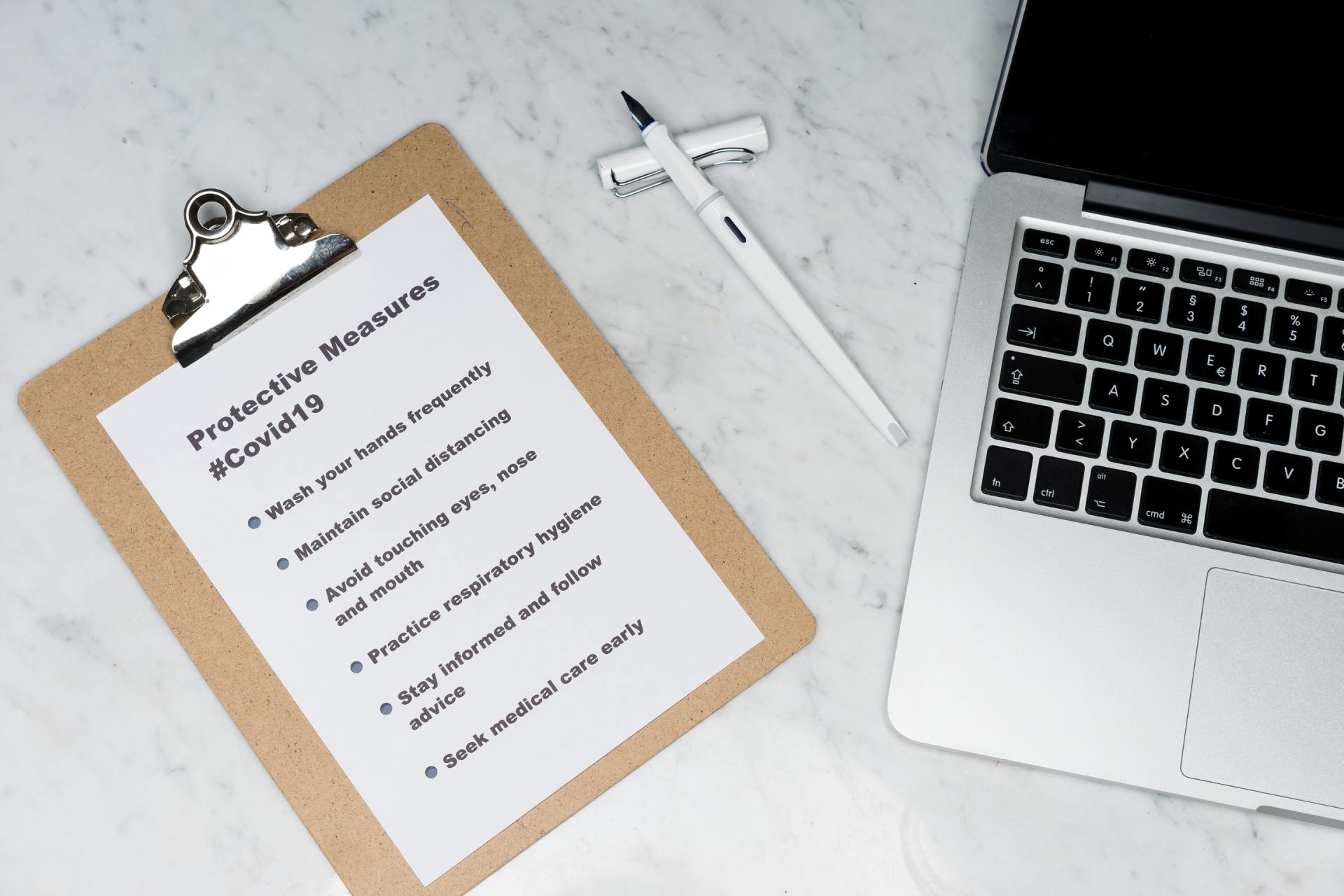
Key points
- Start with small and measurable goals that can be easily attained and used to motivate clinical staff. For example, you can target documentation of indications as an initial priority area.
- Undertake an initial gap analysis, develop a risk register, target key issues and develop an action plan for the AMS program.
- Review existing policies and resources, and identify key groups of stakeholders who can be engaged.
- The risk register should identify and describe current and anticipated risks, mechanisms of accountability and possible countermeasures.
- Select target interventions and communicate appropriately with affected staff and units.
- The AMS action plan should identify and describe the specific activities have been (or need to be) undertaken for the attainment of proposed goals.
Starting a new antimicrobial stewardship program
“Where do I start?” This is a common question to ask when thinking about establishing a new AMS program. It is easy to become rapidly overwhelmed and lose sight of where attention needs to be focused, particularly as antimicrobials are one of the most commonly prescribed agents in hospitals, and they are used by almost every unit and on almost every ward.
Developing a fully functioning, robust and comprehensive AMS program takes time (sometimes years), so there is no need to tackle everything at once. Starting a new AMS program can be challenging. However, establishing a few key structural elements, together with some small interventions and audits is often enough to get an AMS program ‘off the ground’ and provide a sense of satisfaction and motivation in the early stages.
There are a number of comprehensive tools that can be utilised during the formative stages of the program, and they provide a structured framework for the program to focus on what is achievable and important. We highly recommend that these are done within the first year of an AMS program. However, we also acknowledge that these may be overwhelming, and hence recommend starting small so that you don’t become demotivated.
Later modules will describe analytical tools, registers and action plans that should be utilised and developed as an AMS program becomes established.
The best advice would be to engage the right stakeholders early. Gather broad support and ensure that the local opinion leaders are on board. Develop an antimicrobial prescribing policy early to give you a clear mandate for action. Then look at any available data to identify a target issue that you think will be a quick win. Start small. Don’t take on too much. Measure change with small audits done often and trumpet your success.
There are a few key steps involved in getting your AMS service off the ground.
1. Get the attention of the executive and clinical leaders.
- This is a global public health priority.
- Our patients deserve high quality and safe care.
- Everyone else is doing this, and we should too.
2. Gather the right people.
- Know who the opinion leaders are and involve them if you can.
- Ensure AMS is not just an ID/microbiology/pharmacy-driven activity.
3. Formulate a policy early.
- This may explicitly state that the organisation expects high quality care.
- We delegate responsibility to the AMS team to guide prescribers to improve.
- We endorse the concept of restrictions and approvals.
- The AMS team has a mandate to audit and report prescribing behaviour.
4. Look at any data that you have available.
- You might be able to refer to trends in volume or cost of antimicrobials used over time.
- You might have data from a small audit of 10 prescriptions that show lack of indication documentation.
5. Decide on a few target issues.
- Choose something with a simple message that is easy to adopt.
6. Implement something visible – a campaign or tool.
- Have a consistent message.
7. Measure improvement and report your success.
- Small audits may be enough to show change over time.
- Report at unit or ward level if possible.
A structured approach to ‘getting started’ will assist in providing a framework for the program to focus on what is achievable and what is important.
Four tasks are key here.
- Perform a gap analysis: gain an understanding of the areas of need and the resources you have available to help.
- Develop a risk register: assess priorities (what problems are common, dangerous), and what mitigation is available.
- Decide on your target issues: decide on specific campaigns.
- Develop an action plan: decide what you will do and how you will measure it.
Gap analysis
A gap analysis should be performed during the planning stages of an AMS program, prior to its implementation and also periodically thereafter. The main goals of this review are to identify key stakeholders, to identify the resources available for AMS, and to understand any current information about antimicrobial use in the hospital.
A number of activities need to be undertaken as part of the gap analysis.
- Identify and engage a member of senior leadership (executive) to support the AMS program.
- Identify and engage physician, nurse, and pharmacist clinical champions for the AMS program.
- Identify and engage existing groups or committees who might have an interest in AMS. Their responsibilities and reporting structures should be understood as well as how they might impact or interact with AMS work. These can include the AMS, IPC, medication safety and patient safety committees, and other groups such as teams for medical education, nurse education, etc.
- Identify the resource allocation (dedicated staff time) available for the AMS team.
- Identify all existing antimicrobial prescribing and management policies. Review the existence, accessibility and acceptance of the organisation’s antimicrobial treatment and surgical prophylaxis guidelines and clinical pathways to assess whether or not they:
- are consistent and evidence-based;
- reflect agreed best practice, e.g., per national guidelines; and
- specify a recommended agent, dose, route and duration of empirical antimicrobial treatment for the major infection categories.
- Examine any existing sources of information to assist in monitoring progress of the AMS program. Examples include:
- antimicrobial usage or expenditure and trends over time;
- microbiology susceptibility patterns; and
- data from electronic prescribing software if available.
A checklist is provided here that can be used to perform your gap analysis during implementation and also periodically to review change over time.
Risk register
Risk registers are tools that can be used to assist with formal assessments of risks, and, therefore, help to prioritise the actions and guide appropriate allocation of resources.
Risk registers should be much more than just a list of risks. They are intended to be dynamic documents that should support decision-making and assist with communication within the AMS committee and between the AMS committee and the executive.
Risks relating to AMS discussed during AMS committee meetings in response to incidents and new issues as identified through day-to-day activities of the AMS team may need to be added to the risk register.
The risk register should include the following:
- description of the risk;
- date that risk was identified (if relevant);
- risk type or area affected;
- likelihood of occurrence – frequent;
- severity of effect – significant;
- overall assessment – high, medium or low;
- countermeasures or actions to be taken to prevent or reduce the risk;
- responsibility/owner – the individual(s) responsible for ensuring that risks are appropriately assessed and countermeasures are undertaken; and
- status – indicates whether this is a current risk or if risk can no longer arise.
In many cases this can be visually represented as a matrix with colour coding of the high-, medium- and low-risk entities.
Find out what your local priority issues are. This means taking a look at local data. Sometimes these issues are clear to local clinicians, e.g., we prescribe poorly for pneumonia. Where possible, comparison with like facilities can be very enlightening.
Selecting target interventions
The AMS committee is responsible for defining a set of measurable and defined improvements for the program to focus on each year. This should be informed by the risk register. This ensures that the highest-risk issues and/or the commonest problems are being addressed. It should also be informed by the local clinicians to ensure that the issues are seen to be clinically relevant.
A critical part of selecting these activities is to consider the evidence that an intervention that will lead to improvement is available, and that key outcomes of interest can be measured. This allows the AMS team to know whether or not the activities they undertake are leading to the expected improvements.
Use SMART criteria to guide your target issues. That is, be mindful that you select things that are:
- specific;
- measurable;
- achievable;
- relevant to clinicians; and
- time-based.
Example of a target intervention
Improving documentation of the indication for prescription of antimicrobial drugs
This is a good campaign to adopt early as it is rarely controversial. It enables all staff to be involved in management and review of antimicrobial therapy. Doctors, pharmacists and nurses will know the indication and can see where therapy varies from recommendations. Sometimes just encouraging a clinician to commit to the indication for use can challenge them and lead to change – for example:
- A doctor may think: ‘I am selecting antibiotics for pneumonia and yet the chest X-ray is clear; am I sure I want to apply this label? Maybe this is bronchitis instead?’ (The outcome may be that no antibiotic is prescribed.)
- A nurse may say to a doctor: ‘You documented you were treating a urinary tract infection (UTI) but the urine is clear; does our patient really have a UTI?’ (The documented indication allowed the nurse to participate.)
- Pharmacist to doctor: ‘You documented that you suspected meningitis but the dose you chose isn’t what we would usually advise for meningitis. Would you like to increase the dose?’ (The pharmacist can offer helpful dosing advice matched to indication.)
- Pharmacist to doctor: ‘You documented that you chose amoxicillin-clavulanate for community-acquired pneumonia but I notice that the guidelines advise amoxicillin. Should we change?’ (Again, having a documented indication means all team members can participate and support one another to improve care.)
- The patient develops a rash overnight and the covering doctor is asked to select an alternative drug – it can be enormously frustrating if the indication for use isn’t documented. (Why was he receiving cefazolin? If the indication was documented, we would know and could make a safe decision about an appropriate alternative.)
A quick win will motivate people. Think about something easy to measure and check it early, e.g., after the first month.
Providing feedback is an essential part of the improvement process, so always tell people about their success and congratulate them, and even offer recognition where appropriate.
When you pick a campaign, you need to strategise well.
- Be consistent – refer to a few key issues and agreed messages.
- Be visible - emails, poster, lanyard cards, shelf talkers, webpage, etc.
- Access all professional groups – nurse, pharmacy and medical.
- Get other specialist groups on board with owning the campaign – don't take on too much.
- Know the limitations of what is safe. Do not expect a pharmacist or ICP to do AMS without expert medical support from somewhere.
- Some patients are different and will be exceptions.
- Always ask – what unintended harm could I be causing?
- Ask for help, share ideas and adapt from others. Collaborate, adopt and adapt ideas, and implement and transform known initiatives. No need to reinvent the wheel!
- Share resources. Be part of an AMS community – compare. This makes your data more meaningful, and your work has broader impact.
Action plan
The AMS committee should develop an action plan that outlines the actions that are required to achieve the goals. For each action, there should be an allocated owner or responsible person(s). The actions should each be allocated a duration or specified period of time for completion.
An example is provided below:
| Issue | Allocated owner | Actions | Timeline | Outcome |
|---|---|---|---|---|
| Improve surgical antibiotic prophylaxis for cardiothoracic surgeries | Person A | Audit, meetings CTS, new posters, meet theatre, audit | Complete on [date] | |
| Documentation of indication on medical wards | Person B | Intern education, audit, feedback, audit | Complete on [date] | |
| Penicillin allergy de-labelling | Person C | Meet immunologists, develop protocol, train pharmacist | Complete on [date] |
Checklist of key elements for an antimicrobial stewardship program
Here is a checklist of key elements for an AMS program. Use this checklist to plan your program's systems and structure, implementation, and monitoring and evaluation activities.