Antimicrobial Stewardship
Implementing guidelines and clinical pathways
Key points
- A clinical practice guideline is an evidence-based statement that includes recommendations intended to promote organised and efficient patient care.
- Evidence-based guidelines lead to the more appropriate use of antimicrobials, optimise clinical outcomes and minimise adverse consequences.
- The guidelines should be visibly endorsed by key clinician leads, as absence of support will adversely affect implementation.
- A clinical pathway is a tool that describes the steps that should be taken in the care of the patient, including tests that may be required, monitoring and treatment.
- Information from guidelines can be transferred to a clinical pathway which can be available at the point of care to promote guideline uptake.
When antimicrobials are prescribed according to evidence-based guidelines, including drug choice, dose and duration, this will usually lead to the more appropriate use of antimicrobials and can help to optimise clinical outcomes and minimise adverse consequences including development of antimicrobial resistance.
Antimicrobial prescribing guidelines are an essential requirement for AMS programs. They describe evidence-based best practice and provide a standard against which prescribing behaviour can be compared. Evidence-based standard treatment and prophylaxis guidelines provide assistance to clinicians in the management of infectious diseases. They should guide the selection of the most appropriate antimicrobial, to most effectively treat or prevent infection, while discouraging the inappropriate use of antimicrobials.
A clinical practice guideline is an evidence-based statement that includes recommendations intended to optimise patient care and assist health practitioners to make decisions about appropriate healthcare for specific clinical circumstances. They should be developed in a transparent manner with potential conflicts of interest stated. Often, they are developed under the auspices of a professional college or associated.
A clinical pathway is a tool to promote organised and efficient patient care. They should be evidence-based and aim to standardise care processes. In most circumstances, the clinical pathway distils information from clinical guidelines, to make it applicable for use at the point of care. The AMS committee will be responsible for the development, implementation, review and audit of clinical pathways for infections and antimicrobial use with support from the hospital executive.
Development
Development of a guideline can be a major undertaking. It requires that the guidelines authors are skilled in analysis and interpretation of published literature. New information needs to be considered against existing practice. The quality of evidence needs to be examined. National and international groups have now compiled many examples of evidence-based guidelines.
Importantly, evidence needs to be adapted to suit the local context. Key considerations include:
- patient population;
- local antimicrobial susceptibility profile (antibiogram);
- local antimicrobial consumption, costs and availability; and
- surgical procedures performed.
Clinical pathways and clinical guidelines may, therefore, require modifications to the local hospital context. Where there are differences between local guidelines and national guidelines, the evidence base for these differences should be clear. For conditions not covered in national guidelines, organisations should refer to the best available evidence and develop local guidelines appropriate to the local context.
The process of clinical guideline and clinical pathway development for antimicrobial prescribing should involve contributions from infectious diseases specialists and microbiologists, with input from doctors, pharmacists and nurses from the relevant clinical specialty area covered by the guideline. During the development phase, concerns raised should be identified and discussed, and resolutions documented. This will ensure the development process is transparent and has included the relevant stakeholders, including key clinician leads. It is particularly important to establish a sense of ownership from the relevant specialty area early on, as this will have a substantial impact on the success of implementation and uptake by prescribes.
Suggestions for common clinical infective indications appropriate for local or national antimicrobial prescribing guidelines are:
- community-acquired pneumonia;
- hospital-acquired pneumonia;
- urinary tract infection;
- skin and soft tissue infection;
- intra-abdominal infection;
- surgical prophylaxis; and
- sepsis.
Antimicrobial recommendations in guidelines and pathways
Antimicrobial recommendations in clinical infection guidelines and pathways should include a first-line empirical antimicrobial therapy for each common indication, with a recommended second- or third-line therapy choice for simple antimicrobial resistance, allergy or severity of illness.
- First choice antimicrobials are recommended on the basis of available evidence and are usually narrow-spectrum agents with positive benefit-risk ratios and low resistance potential.
- Second choice antibiotics are broader-spectrum with a less favourable benefit-risk ration and higher resistance potential.
Severity of infection should be considered where relevant, to differentiate choices and help optimise antibiotic selection.
The WHO Essential Medicines List includes empirical first- or second-choice treatment options for common infectious syndromes, which can be adapted for local use.
The treatment options recommended should be widely available, at an affordable price, in appropriate formulations and of assured quality. Where possible, recommended antimicrobials should be from the Access group of the Essential Medicines List, with a limited number of Watch group antibiotics recommended for specific indications.
The below is an example only. The recommended empirical treatment choices will be influenced by local or national circumstances, such as the availability of antibiotics and local resistance patterns. They may not apply to a specific patient and should not replace clinical judgement.
| Indication | First choice | Non-immediate penicillin allergy | Immediate penicillin allergy |
|---|---|---|---|
| Mild CAP | Amoxicillin OR doxycycline | Doxycycline OR cefuroxime | Doxycycline |
| Moderate CAP | Benzylpenicillin AND doxycycline | Ceftriaxone AND doxycycline | Moxifloxacin |
| Severe CAP | Ceftriaxone AND azithromycin | Ceftriaxone AND azithromycin | Moxifloxacin |
Implementation
The development of guidelines alone is not enough to achieve effective change and adherence to these can vary between staff in different clinical areas. Guideline development needs to be supported by a program of ongoing educational activities for all relevant healthcare professionals on the need and intended use of the guidelines so as to ensure compliance. Effort is required to promote and encourage uptake of antimicrobial prescribing recommendations in guidelines and clinical pathways. This is the key to translating evidence into practice.
Successful implementation requires the support of motivated individuals to facilitate change. It is essential to understand the existing culture and prescribing practices of the organisation, the drivers affecting these, and any potential barriers or enablers to effect change. Importantly, the workflow of the staff involved also needs to be understood, so that opportunities to guide change are identified. The AMS team may need to visit relevant hospital departments and attend unit meetings to discuss the guidelines, to promote awareness and ensure that they are appropriate for the local context.
The guidelines should be visibly endorsed by key clinician leads, as absence of support will adversely affect implementation. Where possible, the guideline promotion should be led by the relevant specialty team (e.g., a surgical prophylaxis guideline is likely to be more successful if openly endorsed by the surgical team).
The implementation process needs to include audit and feedback to inform implementation planning and promote uptake. Evaluating the use of prescribing guidelines can help to identify whether implementation strategies are effective and whether alternative approaches are needed. This will help understand reasons for non-compliance with the recommended guidelines, assist with future improvements to these guidelines, and enable unintended consequences to be identified and addressed. Clinical staff should be educated about the need for prescribing guidelines, and informed that they have been specifically developed to suit the local context and should, therefore, be trusted. This education should also include sample content of the guidelines, with clinical scenarios and case-based examples to work through to help demonstrate their clinical relevance and intended use.
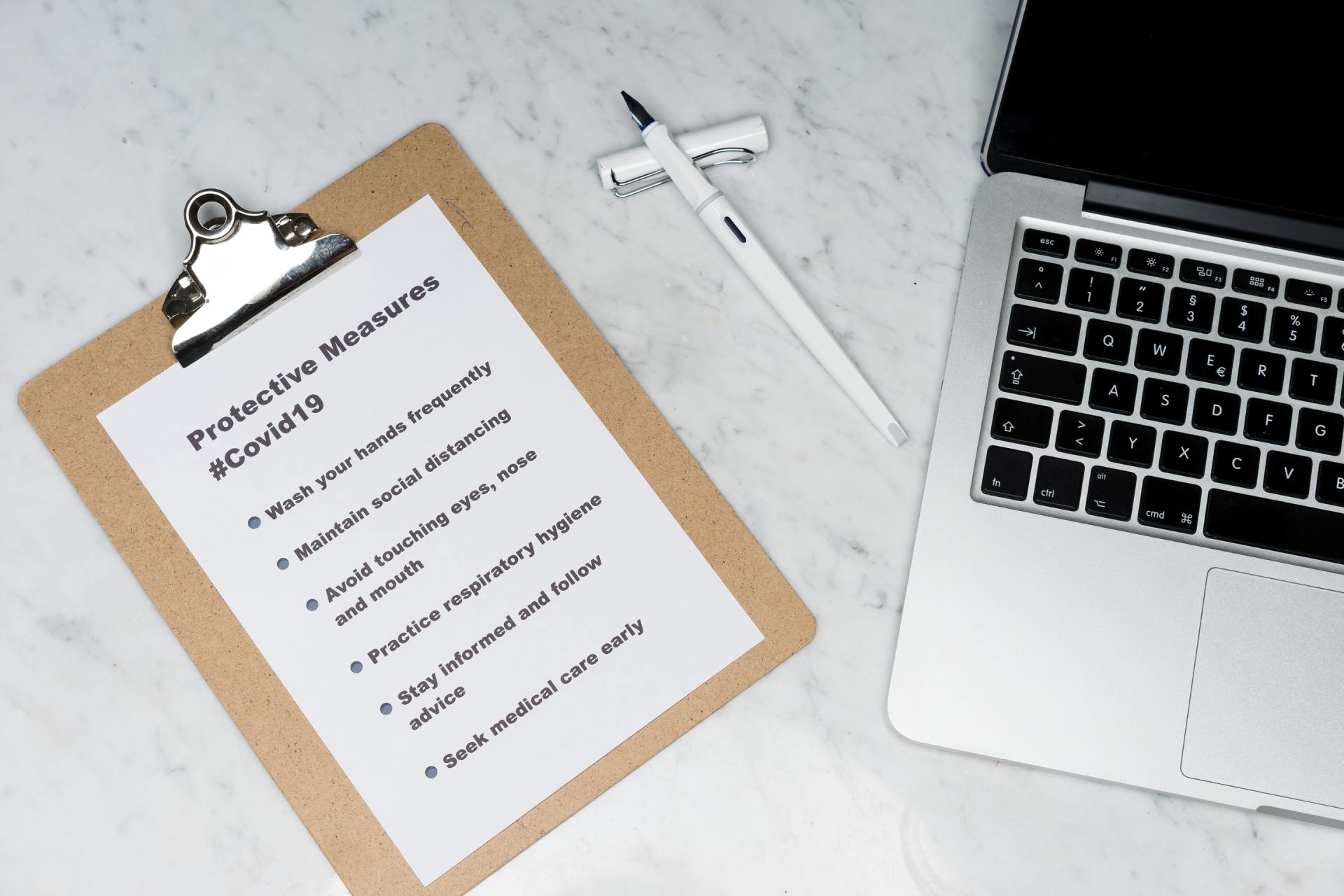
Tools to support guideline implementation
Clinical pathways
Information from guidelines can be transferred to a clinical pathway which can be available at the point of care to promote guideline uptake. A clinical pathway is a tool that describes the steps that should be taken in the care of the patient, including tests that may be required, monitoring and treatment.
Clinical pathways have been used by doctors, nurses and pharmacists in hospital and community settings to help standardise patient care and promote optimal antimicrobial prescribing. They can be particularly useful in a busy environment (e.g., elective surgical procedures with predictable clinical courses), as the pathway can direct appropriate decisions in a step-wise, structured fashion.
Clinical pathways for the management of pneumonia, for example, have been shown to improve the appropriateness of investigations ordered and empirical antimicrobials prescribed. They may also direct the prescriber as to when to routinely consider de-escalation or cessation of therapy, or if it may be appropriate to switch from the intravenous to oral route. Such clinical pathways can, therefore, help to encourage the more appropriate choice, route and duration of antimicrobial therapy.
Sepsis pathways are another example of a clinical pathway with a series of steps to be followed in real time while managing patients with this condition. It should drive prescribers towards appropriate empiric drug choices as well as guiding relevant investigations.
The AMS team can promote the existing clinical pathways, educate staff, and liaise with hospital executive to secure endorsement. They should also ensure that these pathways are readily available at the prescriber’s point of care, preferably through several sources. These may include pocket-sized printed edition or electronic versions, e.g., though the hospital intranet or possibly though other technology such as smart phone applications. Posters, checklists and visual aids available at the point of care and specific to the local context can also promote guideline uptake.
Other tools
Lanyards and posters, screensavers and shelf talkers are all tools that can be used to help implement the information provided by a guideline at the point of patient care. It is important that the information is consistent and seen to be endorsed by the organisation. For example, booklets and lanyards may be provided to new medical staff. Posters may be located in appropriate locations, e.g., surgical prophylaxis recommendations in theatre. Posters about intravenous to oral switch may be located in medical wards. More information about these strategies is discussed here.
Maintenance
Clinical pathways should be reviewed and updated regularly by the AMS team in consultation with key specialty clinicians to ensure that evidence-based best practice is maintained at all times. A review at least once per year is recommended, with the team needing to consider the latest national guidelines (if available), and local microbiology and resistance patterns. The AMS team's contact details should be provided on guidelines and clinical pathways so that prescribing staff can ask questions and provide feedback on the content, ensuring that criticisms or suggested improvements are considered for future updates. It is important that only the latest versions of guidelines and clinical pathways are available for use.
Examples of guidelines and pathways for common scenarios
Surgical antimicrobial prophylaxis
Surgical prophylaxis represents a common indication for antimicrobial use in the hospital setting. Therefore, ensuring appropriate surgical antimicrobial prophylaxis (SAP) prescribing is an important component of an AMS program. Guidelines should encompass the key elements of appropriate SAP including:
- correct indication;
- antimicrobial choice;
- dosage;
- route of administration;
- timing of administration; and
- duration.
Each of these elements must be considered at the point of prescription, review and assessment.
| Element of SAP prescribing | General recommendations |
|---|---|
| Indication | Clean-contaminated procedures, contaminated procedures, operations involving the insertion of an artificial device or prosthetic material |
| Antimicrobial | 1st-generation cephalosporin, e.g., cefazolin |
| Dose | Drug dependent, e.g., 2 grams cefazolin |
| Route | Intravenous |
| Timing of administration | Within 60 mins prior to surgical incision |
| Duration | Single dose |
Confer with guidelines for more specific recommendations per surgical procedure.
Sepsis is one of the leading causes of death in hospital patients worldwide. Appropriate recognition and timely management of patients with severe infection and sepsis is a significant challenge. Delayed treatment is associated with higher mortality rates, significant morbidity and high costs to the healthcare system.
The purpose of a sepsis pathway is to ensure the early and optimal recognition and management of septic patients. It seeks to translate evidence-based clinical guidelines for sepsis identification and treatment into practice, educate clinicians, promote improved patient outcomes, and enhance patient safety.
The goal of a sepsis pathway is to reduce the:
- time to administration of antimicrobial therapy;
- number of intensive care unit admissions;
- lengths of stay;
- use of last-line antimicrobials; and
- mortality of septic patients.
A sepsis pathway can be implemented for use in emergency departments as well as on inpatient wards.
The pathway should include, but is not limited to:
- information on recognition of sepsis: risk factors, signs and symptoms;
- information on resuscitation with rapid intravenous fluids and antibiotics within the first hour of recognition of sepsis;
- instructions about other actions, including administering oxygen if necessary, taking blood cultures and measuring serum lactate; and
- instructions about referral to senior clinicians and specialty teams as required.
Selecting the right antimicrobials and doses to prescribe is crucial, so pathways should include recommended antimicrobials for sepsis of unknown source and for suspected sites of infection. The recommendations should be based on national guidelines or local AMS endorsed guidelines and should be readily available at the point of care, e.g., within the pathway itself.
Sample checklist for developing a new clinical pathway
Planning phase
- The AMS Committee will be responsible for deciding which condition requires a clinical pathway. They should be involved in the development, implementation and review of the pathway.
- The AMS team can make a recommendation to the Committee that a new pathway be developed, based on areas of deficient practice that they have seen on the ward.
- If there are a large number of pathways that need to be developed, it may be useful to write one at a time, rather than attempting to tackle them all together.
- Nominate a core writing group of clinicians that have adequate knowledge in the clinical area and are able to review and interpret the evidence base. There should be input from doctors (including an infectious diseases specialist and or clinical microbiologist), pharmacists and nurses or infection control practitioners.
- It is important to involve clinicians belonging to the clinical specialty that the pathway is focused on, or a group that the new pathway will have a major impact on. For example, if developing a pathway on the management of community-acquired pneumonia, it would be prudent to involve members of the respiratory unit, emergency department and/or general medicine unit.
- Determine what the scope of the pathway will be. Will it only comprise of treatment recommendations, or will it also include diagnostic workup?
Writing the pathway
- Review the evidence:
- Determine the evidence base that the clinical pathway will be based on.
- For the majority of common clinical conditions, there is likely to already be a national or international guideline in existence, which will be a useful started point. For example, the WHO provides a Model List for Essential Medicines, which should be adapted for local use.
- It is important that your local hospital pathway is written to suit your local context, including:
- the patient population;
- local antimicrobial susceptibility profile (antibiogram);
- local antimicrobial consumption, costs and availability; and
- if relevant, the surgical procedures performed.
- Importantly, where the local hospital pathway differs from an existing guideline, the reasons for this should be clearly documented.
- Write the pathway:
- Ensure the pathway is written in a clear and logical manner with simple language.
- The pathway may include the following areas
- target audience/ the patient group that the pathway applies to;
- definitions of acronyms;
- definition of the clinical syndrome;
- clinical assessment criteria including signs and symptoms;
- other diagnostic considerations including routine investigations (microbiology, pathology and radiology) or any relevant scoring systems (e.g., CORB for community acquired pneumonia);
- the role of allied health (e.g., physiotherapy assessment);
- antimicrobial recommendations: the pathway should recommend first-line empirical antimicrobial therapy, with a second- or third-line therapy choice to cover scenarios such as simple antimicrobial resistance, allergy or severity of illness. Recommendations should include antimicrobial choice, dosage, route, dosing frequency, administration instructions (e.g.; for an IV infusion), suggestions for de-escalation or oral switch (if relevant) and duration of therapy.
- any supplementary non-antimicrobial therapy such as fluid replacement; and
- recommendations for follow-up.
- You may also consider writing an information leaflet to be provided to the patient or carer explaining the condition, the treatment they are receiving and any additional instructions to help manage their condition.
- Ideally, the pathway should have areas for clinicians to sign and date once each task has been completed.
- If there are differences of opinion that arise during the development of the pathway, ensure these are documented so that they can be referred to at a later stage if required.
- The pathway should be reviewed by at least 1-2 people who are not part of the core working group to ensure that it is clear, feasible and practical.
Implementing the pathway
- Appoint a clinical champion, ideally a senior medical clinician from the specialty most relevant to the new pathway. They should be visibly endorsing the pathway and leading by example.
- Schedule meetings with medical specialties, wards and/or individual clinicians to promote awareness about the new guidelines and ensure that they are relevant and practical for the local context.
- As part of your communication strategy, ensure clinicians understand that the clinical pathway has been adapted to suit the local hospital context.
- Ensure the pathway is easily visible and accessible at the point of care. For example, posters, pocket-sized printed editions and printed copies may be made available on the wards, and electronic copies may be made easily accessible via a computer or mobile device. In the case of a new surgical prophylaxis pathway, you may wish to format it into a poster that can be displayed in theatres.
Evaluating the pathway
- Regular auditing and providing feedback to the relevant clinicians is a key aspect of successful implementation. There are a number of options for doing this:
- If there is a PPR service in place, you may wish to incorporate feedback at the point of patient review if the patient’s therapy is not consistent with the pathway recommendations.
- Conduct regular, small quality audits on the wards with patients who are most likely to be affected by the new pathway.
- Wherever a patient’s therapy is found to be non-concordant, a discussion should be had with the treating medical team to determine the reasons for this and whether the pathway needs to be modified to better suit the clinical context and workflow.
- It is important that the AMS team is aware of any potential negative impacts of the new recommendations and hence should monitor for harms.
- The pathway should be reviewed, ideally every 1-2 years, to ensure the content is still clinically relevant in light of any new published literature or new international or national guidelines.