Antimicrobial Stewardship
Feedback and communication
Key points
- Regular reporting of information on antimicrobial use and resistance to relevant stakeholders is an essential element of a successful AMS program.
- Different stakeholders will require feedback and communication about different types of information that is gathered by the AMS team.
- When data or audit results are communicated, interpretation of the information needs to be provided at the same time.
- Finding the best mode of feedback for each stakeholder group can be difficult and may require creative methods.
- It is important to understand the needs and requirements of both the feedback provider and recipient, and the interaction between the two groups.
Regular reporting of information on antimicrobial use and resistance to relevant stakeholders is an essential element of a successful antimicrobial stewardship program. The information that is provided should be meaningful and drive action in the institution. It should highlight areas of high risk or poor performance, as well as areas of good performance. This peer level benchmarking can be very effective.
It is also important to recognise that AMS straddles several areas of quality improvement in the hospital, including infection prevention, medication safety, and management of the deteriorating patient (e.g., sepsis). AMS information is relevant to all of these areas, and hence there is often a significant burden of data collection and auditing placed upon poorly resourced AMS programs.
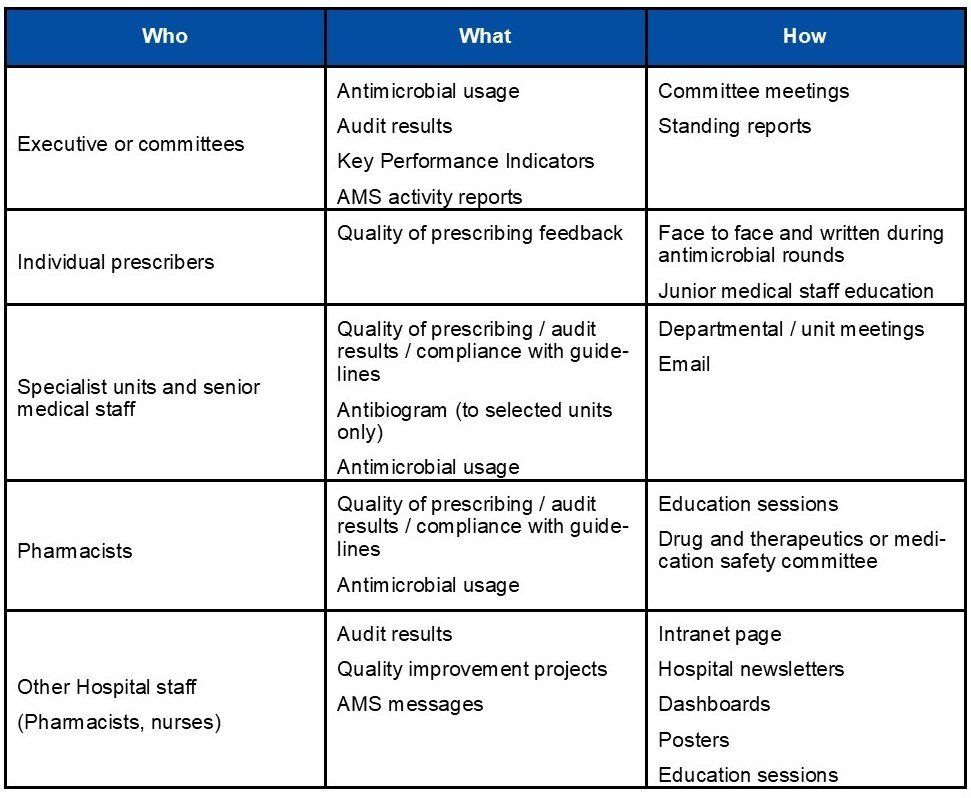
Who to provide feedback to
AMS teams or committees may be required to report to numerous stakeholders including:
- national programs such as those involved in hospital accreditation;
- hospital executive or senior management;
- relevant hospital committees, such as drugs and therapeutics (DTC), patient safety and infection prevention committees;
- heads of specialty units and senior doctors;
- individual antimicrobial prescribers;
- pharmacy; and
- nurses.
What needs to be reported
Different stakeholders will require feedback and communication about different types of information that is gathered by the AMS team. It is important to compile and only report on the data that is relevant to the given group, so as to highlight the important information that you want them to understand and act upon.
Examples of information that could be communicated to stakeholders include:
- antimicrobial usage data at the hospital, ward or unit level, and usually presented over a time-period by month
- this type of report requires data extracts and manipulation from pharmacy systems;
- antimicrobial resistance rates and antibiograms
- this requires detailed data about clinical isolates from the institution and may not be available in sites that do not have a laboratory or access to AMR surveillance programs;
- point prevalence surveys of antimicrobial use and indications and infections;
- quality of prescribing audits (i.e., appropriateness of use);
- results of quality improvement audits;
- other current improvement initiatives in the organisation such as clinical guideline or pathway implementation;
- activities of the AMS program, including education initiatives and activities (such as the number of AMS rounds, patient reviewed, interventions);
- educational messages; and
- antimicrobial shortage alerts.
When data or audit results are communicated, interpretation of the information needs to be provided at the same time. Each report or communication should include:
- suggested actions for improvement;
- targets or goals;
- comparison with previous audit results to demonstrate any change in practice; and
- benchmarking or comparisons if possible, e.g., compare with other units, other hospitals in the region.
How to provide feedback
Finding the best mode of feedback for each stakeholder group can be difficult and may require creative methods. In LMIC countries that have limited information technology infrastructure, access to electronic sources such as emails, pagers, intranet websites will pose a challenge. AMS experts in these countries look to smartphones as a potential medium.
Where possible, feedback should be incorporated into existing unit, executive or leadership meetings so that senior staff (who are the decision-makers) are exposed to the reports. For junior medical staff, workforce rotations are common, so effort should be made to repeat communication regularly.
In LMIC hospitals, opportunities for establishing a program that engages nurses in AMS may be limited due to nurses’ workload, and the culture and hierarchies in place. Nevertheless, educational opportunities and feedback that highlights key areas of action are important to pursue.
Feedback and AMS information can be communicated via a range of methods and through various forums, depending on the target audience. Several strategies are likely to be necessary to disseminate all the data.
For feedback to be effective, it is important to consider the following features; feedback should:
- contain specific information rather than generalisations;
- be accurate and clear;
- be objective (unbiased and unprejudiced);
- be given in a timely manner (as soon as possible after completion of a task);
- be associated with core AMS goals so the individual can improve performance;
- provide a feature that is desired by the receiver; and
- be clear and concise to ensure the most effective feedback.
Mediums for feedback include:
- e-mail;
- committee meetings
- reports can be tabled at the relevant hospital committees preferably as a standing agenda item;
- face to face at education sessions, unit or department meetings;
- posters;
- dashboards in ward areas;
- newsletters;
- hospital intranet page;
- hospital grand rounds; and
- morbidity and mortality audits.
When providing feedback on antimicrobial stewardship initiatives, it is important to ensure that this is done in a manner that encourages improved prescribing. To facilitate this, begin with any positive feedback first, then introduce the constructive or negative feedback and end with specific aspects that could have been done differently to ensure compliance and appropriateness.
Feedback and information can be coupled with general AMS education, so that the receiver of feedback feels they are gaining more from the discussion. Workforce rotations are common in many settings, so effort should be made to repeat this education and communication regularly.
When providing feedback to different groups, it is important to understand the needs and requirements of both the feedback provider and recipient, and the interaction between the two groups. To improve this relationship and to get the most out of any interaction, it is important to ensure that:
- the feedback provider is credible and trusted by the feedback recipient;
- the timing and circumstances of the feedback are appropriate;
- the feedback message is clear and helpful to the recipient;
- the feedback is conveyed with good intentions; and
- the feedback is given in an interactive manner.
Although it is often tempting to provide feedback and education on many aspects of your program while you have the opportunity, it is often more effective to limit these to only a few key issues or messages that you wish to convey. This will have greater impact and highlight those issues that you feel are the most important or are able to be acted upon by the group you are addressing. Another option is to provide a summary of the key issues that you wish to highlight (say, three) at the end. This will again bring the critical or achievable items together in the form of an easily actionable list.
Executive or committees
Reports should be created in a way that is easy to follow and read, without too much detail. The main important messages need to be the focus of the report. Reports should be regularly shared with hospital executive and relevant committees, and these reports could contain:
- antimicrobial usage data (can be broken into ward or division);
- audit results on quality of prescribing;
- key performance indicator results; and
- AMS activity and progress reports.
One way to share this information may be to table these reports at committee meetings, e.g., DTC, infection prevention committee, AMS committee, etc. If possible, include an AMS report as a standing agenda item for committee meetings with key stakeholders.
Individual antimicrobial prescribers
Feedback about how prescribers can improve their antimicrobial prescribing should be directed to the prescriber immediately after a review of an individual episode of prescribing has been completed during the post-prescription review process. Ideally, this would be face-to-face to allow discussion and queries about the advice. Documentation of the feedback and advice should also be included in the patient medical record.
Specialist units and senior medical staff
Measurement of the quality of prescribing, including data on compliance with guidelines, should be regularly reported to prescriber groups. The clinical workforce needs feedback on their performance, ideally relative to other units and wards, or to other hospitals. Presenting locally derived, meaningful data to small groups of clinicians (e.g., at departmental meetings) is likely to be more successful than emailing formal reports.
Feedback sessions can be tailored for the target audience and include the results of the audit and discussion around relevant guidelines and evidence, to educate hospital staff on best or accepted practice.
The most current antibiogram (with interpretation) should be distributed to the relevant prescribers at your facility but not to all clinicians. Examples of specialist units that may receive the antibiogram are infectious diseases clinicians, intensive care unit and haematology unit.
Antimicrobial usage data broken into units with comparisons may also be useful to email to senior medical staff or discuss at departmental meetings.
General hospital staff
General hospital staff includes junior doctors, pharmacists, nurses, etc. They could be provided with:
- information about quality improvement projects happening in the organisation and in their area;
- results of audits relevant to their practice area;
- information on AMS related topics in hospital newsletters and intranet pages; and
- posters on wards.