Antimicrobial Stewardship
Scope
This webpage has been designed to outline the core principles of AMS that may be used in the implementation of a new or existing AMS program.
The primary objective is to provide a framework to help guide primarily acute care facilities in developing structures and governance for AMS, and outlining the education, training and resources required for an effective AMS program. This information has been written based on experience of implementing AMS in Australian hospitals. As such, it may be most relevant to hospital-based staff; however, it can be used by people in other settings. The secondary objective is to provide suggested strategies with known success in influencing behavioural change around antimicrobial prescribing practices and in reducing inappropriate use.
A third objective is to outline the core components of an AMS program that may be implemented as part of minimum standards for hospital accreditation. These components could be assessed by a national credentialing body, to ensure compliance with standards and allow formal registration.
AMS must be embedded in everyday hospital practice. Thus, it needs to be practical and generalisable to ensure sustainability. There is no singular correct way to implement and sustain a hospital AMS program. Every hospital will likely develop a program unique to their facility’s case mix, available resources and local issues.
Our modules here provide a list of potential strategies and suggested components of AMS programs that each facility may choose to adopt and refine as they see fit. There are some components that are essential and have proven success as parts of effective AMS programs, and we strongly recommend that these are implemented; there are other components that may be adapted if there is a clinical need and if adequate resourcing is available. This is by no means an exhaustive list of potential strategies, and other potential strategies should be developed and adopted according to local requirements.
This information been written and compiled by a multidisciplinary team of experts, including infectious diseases doctors, clinical microbiologists, pharmacists and nurses. The information and resources provided are based on the many years of experience that members of the team have accumulated from developing, implementing and managing AMS programs. As such, we understand the need to adapt AMS programs to suit a variety of different settings.
This page is not intended to be a definitive resource for implementation of AMS programs within all facilities. Rather, it aims to provide information on a structural framework around which an AMS program can be locally developed. It should help to generate ideas and educate those new to AMS regarding the core and desired components that are necessary for effective AMS implementation in acute care facilities.
The authors are aware and acknowledge that evidence changes over time and the ideas and material presented in this publication will evolve rapidly. Importantly, it is expected that this document will require customisation by local or regional experts to suit the individual hospital’s context. While all AMS programs will continue to develop and mature over time as ideas are refined, and as we learn from one another and share success stories, it is important to remember that innovation and flexibility will remain crucial.
Areas out of scope
AMS cannot be implemented, within a facility or as part of a national action plan, in isolation and be expected to have a major impact on AMR within the region. The threat of increasing AMR cannot be effectively managed within a country or region without a multifaceted solution. Only with an integrated framework of programs and activities, including AMS programs, infection prevention and control (IPC) programs, national surveillance programs, effective medication management systems and regulation of the pharmaceutical industry, can a truly robust and effective systems approach to combatting this growing international threat be realised.
Components that are out of the scope of this document are those issues relating to AMR that are required for an effective AMS program but are outside its scope, or those that need to be resolved on a national level and cannot easily be addressed by individual facilities.
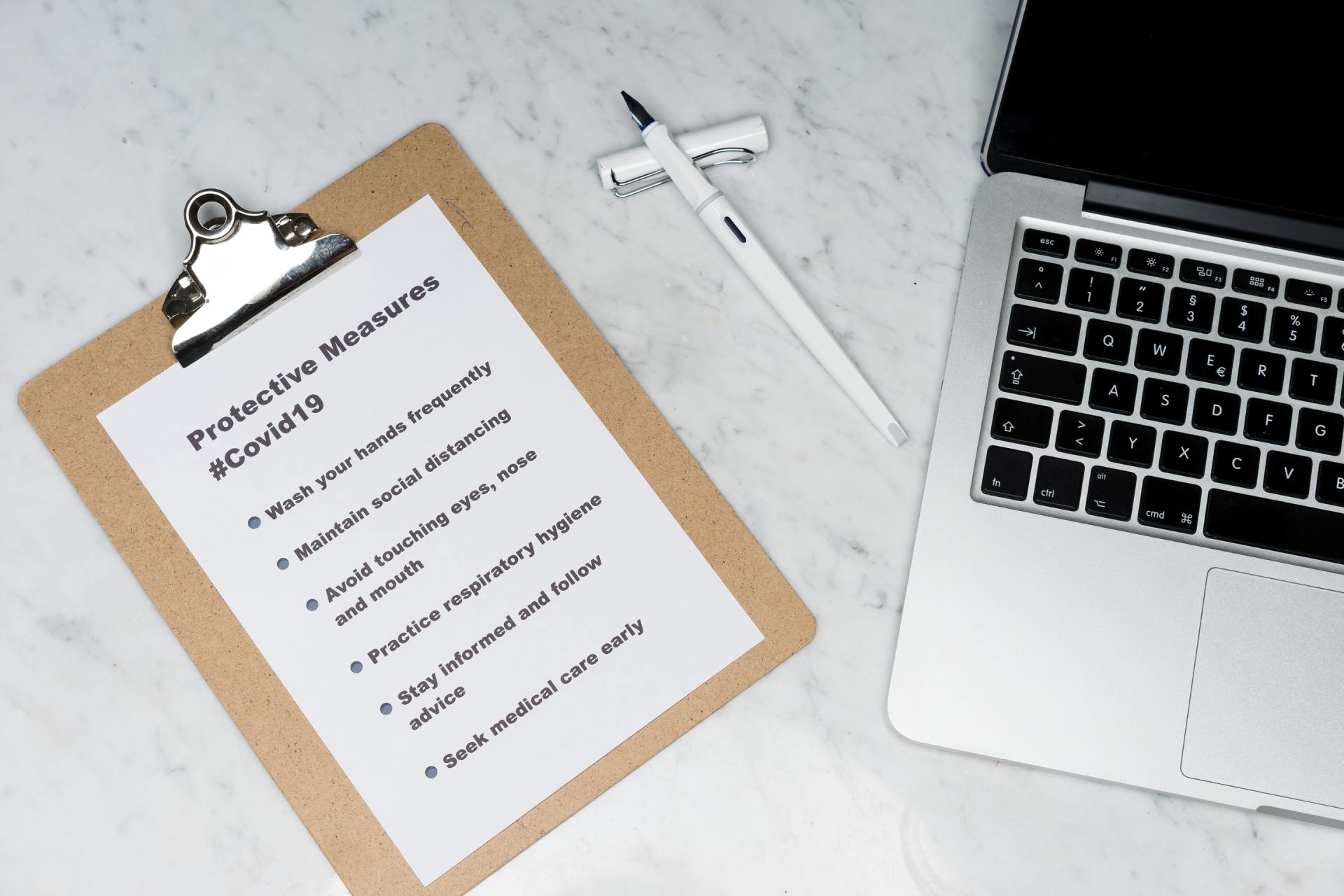
Infection prevention and control
Although it is not the focus of this module, infection prevention and control (IPC) plays a critical role in the prevention of transmission of multi-drug resistant organisms (MROs), both locally and nationally. AMS is unlikely to be successful in containing AMR without robust IPC.
IPC-related issues pose particular barriers to effective control of AMR in acute care facilities in LMICs. These may include:
• large open wards, with high numbers of patients;
• ward crowding due to the presence of family members;
• nurse-to-patient ratios of up to 1:25;
• shortage of trained IPC staff;
• inability to effectively cohort patients colonised with multi-resistant organisms (MROs);
• lack of effective communication and documentation about MRO colonisation in patients who are readmitted or transferred from other sites;
• the aging infrastructure of buildings and equipment;
• variability in the placement and availability of alcohol-based hand rub solutions; and
• lack of monitoring of cleaning quality.
The WHO has published its Guidelines on Core Components of Infection Prevention and Control Programs, and this document should be consulted while developing an IPC program. Documents advising on IPC and AMS should be used together when developing an effective program to combat AMR within a facility.
Availability of antimicrobials without a prescription
Although the sale of antimicrobials without a prescription is now illegal in most countries, it is still often possible to obtain these agents over the counter from some community pharmacies. Hospitals that experience regular stock shortages may rely on the ability of family members to purchase these medications to meet the shortfall. Although there is the understanding that many people without access to doctors, due to either remoteness or social inequality, rely on their ability to access such medicines through pharmacies without a prescription, this access issue will need to be addressed through national policies restricting over-the-counter access to antimicrobials and will not be covered in these guidelines.
Pharmaceutical industry
There should be a national policy restricting the ability of pharmaceutical companies to provide inappropriate financial incentives to doctors and pharmacists. Regulating the pharmaceutical industry with a code of conduct for how they can interact with prescribers and reducing their ability to provide financial initiatives to both hospitals and prescribers for using their antimicrobial medications may encourage more appropriate prescribing of antimicrobials.
Counterfeit and unregistered medications
The presence of counterfeit medications has been acknowledged; however, it is not deemed to be a widespread issue. It has been estimated that the prevalence of counterfeit medicines in the market was 3-5%, although in some settings this may be as high as up to 30%. This will need to be addressed as these agents may be of reduced quality, have lower efficacy, lead to poor patient outcomes and contribute to the development of AMR.