Antimicrobial Stewardship
The antimicrobial stewardship team
Key points
- The AMS team manages the hospital’s AMS program at a day-to-day level and is responsible for enacting the strategies to achieve the goals determined by the AMS committee.
- The team should be multidisciplinary.
- Core members should include a doctor and a pharmacist or nurse.
- A substantial proportion of AMS can be performed by non-expert professionals who receive some basic training in AMS.
- If specialist infectious diseases personnel are not available within a hospital, the team should identify how off-site specialist advice can be accessed.
- Team members should have dedicated time for AMS activities, although time allocations can be shared across a group of clinicians from each profession.
- The roles and responsibilities of the AMS team include implementation, education, monitoring and reporting of AMS activities.
The AMS team manages the hospital’s AMS program on a day-to-day basis. The AMS team is distinct from the AMS committee as the AMS team is responsible for enacting the strategies to achieve the goals determined by the committee. The team report to the AMS committee (or equivalent), although, in practice, members of the AMS team will usually be part of the AMS committee.
Most large hospitals will have a local AMS team on site. In smaller hospitals, the AMS team may take responsibility for acting across several sites (e.g., as part of a larger hospital network). Where a network AMS team is in place, each hospital should at least have a local AMS ‘champion’ on site; that is, a local person who can be a familiar face to local staff and communicate between the AMS team and the clinicians.
Who makes up an antimicrobial stewardship team?
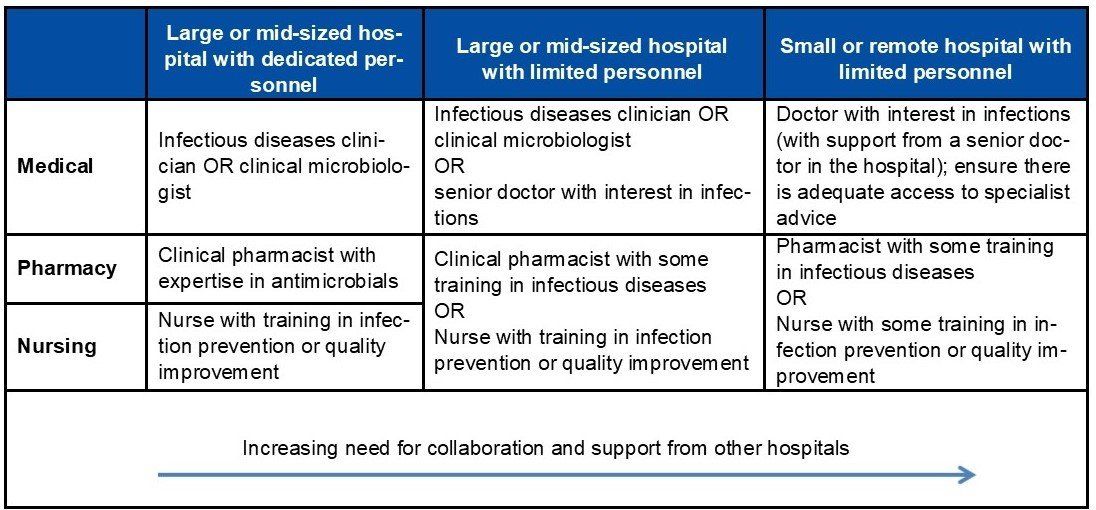
This team should be multidisciplinary, although the exact composition will vary and depend on each hospital’s resources and the nature of the patients who are being managed there. An AMS team does not necessarily need to be large and complex in order to be effective.
When recruiting staff to form an AMS team, consideration should be given to each member’s strengths, skillset and differing perspectives to understand their potential contribution. Members of the AMS team should be familiar with clinical workflows so that their advice is practical, feasible, and sustainable, and they should be adequately experienced to have credibility with staff. They should also possess good communication skills and be flexible to adapt strategies to suit different contexts.
At a minimum, the core AMS team should comprise:
- a doctor (an infectious diseases clinician or doctor with an interest in infections or antimicrobial use);
- and a pharmacist or a nurse.
The following ‘expert group’ members are desirable, but not essential:
- infectious diseases physician;
- clinical microbiologist;
- clinical pharmacist with knowledge of antimicrobials; and
- infection control practitioner or specialist nurse.
A significant proportion of AMS can be done by non-expert healthcare professionals if they receive basic training in AMS. For example, nurses and pharmacists can manage most of the AMS team's activities as long as adequate support is provided and structured discussions with medically trained staff are in place to confirm advice given for more complex patients. Similarly, physicians, surgeons and general practitioners can play active roles in AMS teams. However, there are likely to be situations where specialist advice is still required (e.g., for patients with complex infections or complex antimicrobial regimens).
It is important to note that AMS activities should not only be the responsibility of the AMS team members. Rational and appropriate antimicrobial prescribing and use is the responsibility of all healthcare professionals; hence, AMS should be built into the day-to-day work of every doctor, pharmacist and nurse in the organisation. Healthcare professionals can practise elements of AMS whenever an antimicrobial is considered, prescribed, dispensed and administered, or its effects are monitored. The AMS team members, however, have dedicated time to conduct organisation-wide activities to promote better practice.
Access to off-site expert advice
Antimicrobial prescribing is a complex activity, and from time to time input from experts will be needed. If specialist personnel are not available on-site at a given hospital, then careful consideration should be given to identifying how the AMS team can access specialist advice when required.
Ideally, this pathway for seeking expert advice should be clearly documented and agreed to by both parties to ensure that lines of responsibility and accountability are clear. It is important that team members do not seek expert advice from different sources at different times, which can lead to confusion, lack of consistency, poor continuity of care and higher potential for error. Having clarity around access to expert advice means that the local team have confidence in knowing that the advice provided is safe and consistent, and that there will be appropriate follow-up (for example, to check the patient's progress on empiric therapy and help adjust treatments over time).
The nominated expert advisors should be familiar with the clinical context for which they are giving advice and also know the hospital well enough to understand the resources it has available and which conditions can be safely managed there.
In a networked AMS model, the expert advisors should also be familiar with the policies that exist (as they would be consistent across the network), and, therefore, understand the constraints within which they are working. Ideally, the expert clinician should also visit the site on a regular basis (for example, monthly or 3-4 times per year) to build rapport and gain a greater understanding of the personnel, patient mix and resources available at the hospital. These in-person visits could also be supplemented with regular contact using video-conferencing, telehealth and/or webinars. At a minimum, phone and e-mail contact should be maintained at all times to provide day-to-day support and advice.
It is also important that a system is in place to document these discussions so that any clinician involved in that patient's care can see the advice given and by whom.
Adapted from: Antimicrobial stewardship teams & committees factsheet, NSW Clinical Excellence Commission
Time allocation
It is vital to gain executive support to ensure that team members have dedicated time for AMS activities. This allows personnel to develop expertise in this area, which will enable meaningful and sustained improvement in care. AMS is critical to high-quality safe healthcare delivery, and hospitals cannot simply rely on the goodwill of healthcare professionals to implement and sustain an AMS program.
Some suggested staff resource allocations are:
- Large hospital (>350 beds): full-time doctor and at least one full time clinical pharmacist or nurse. Hospitals with more than 500 beds are likely to require a team of pharmacists or nurses.
- Medium hospital (100-350 beds): part-time doctor and full-time clinical pharmacist or nurse.
- Small or remote hospital (<100 beds): part-time doctor and part-time pharmacist or nurse.
Doctors, pharmacists and nurses may elect to share the time allocations using a rostered arrangement across a group of clinicians from each professional group. For example, several doctors may share a full-time role (1 full-time equivalent [FTE]), thus distributing the responsibilities and taking advantage of different perspectives and skillsets. They may then allocate the remaining time to other responsibilities such as infection prevention duties, clinical ward service, administration, research duties or medication safety.
Previous publications have described resource allocations in various countries; however, what has been allocated and what is actually necessary may differ substantially. Hence, it is important that each hospital allocates resources based on their own individual circumstances and commits to continually reviewing this allocation.
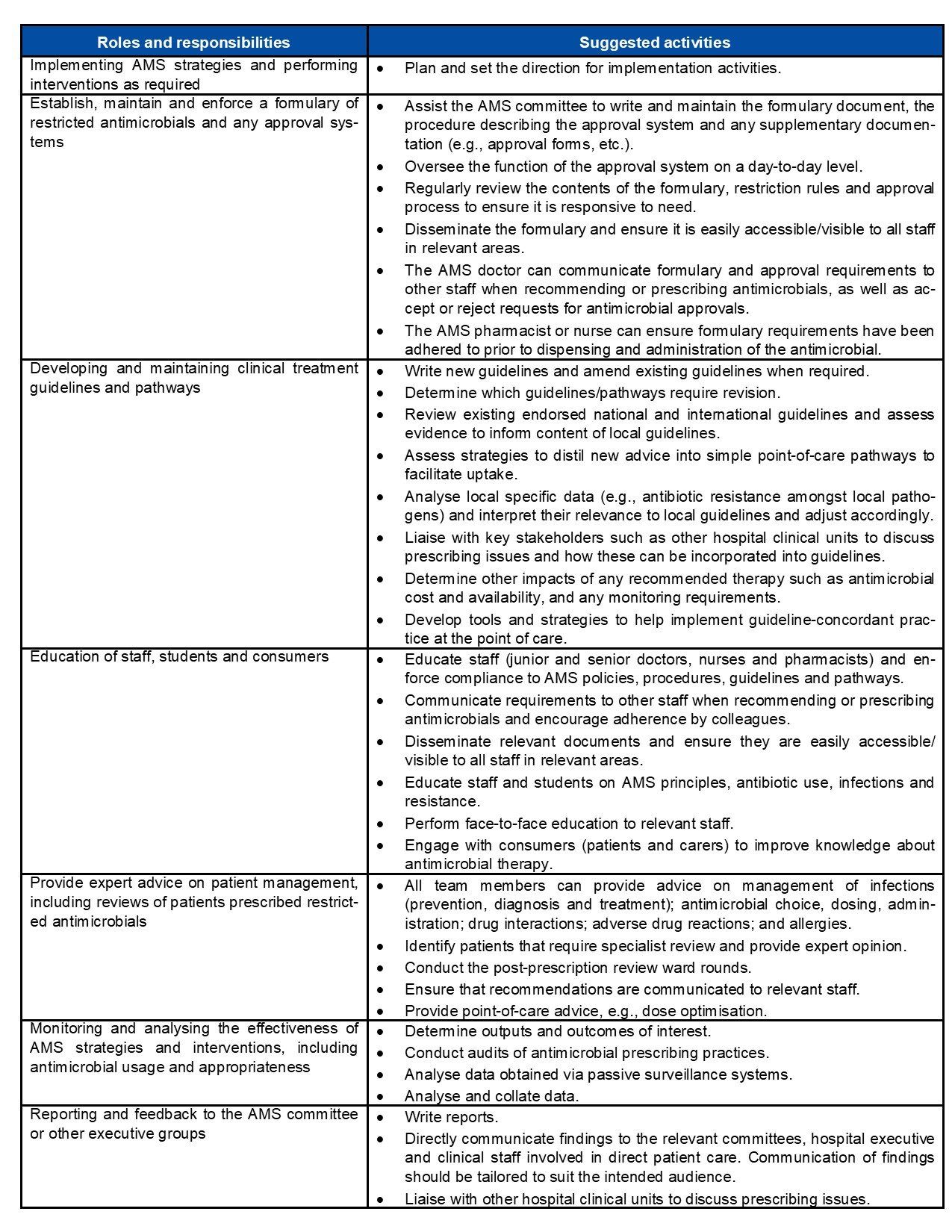
Roles and responsibilities of the antimicrobial stewardship team
The roles and responsibilities of the AMS team include implementation, education and enforcement, and monitoring and reporting of AMS activities. The team's activities are likely to include several different complementary strategies, and are further outlined in Table X.
The team report to the AMS committee (or equivalent). The AMS committee will set the goals and priorities, and write the policies and procedures to assist the AMS team. The AMS team then plan and implement the activities in order to achieve the desired changes in antimicrobial prescribing. The impact of these activities should always be measured and reported.