Antimicrobial Stewardship
The role of the clinical microbiology laboratory
Key points
- The clinical microbiology laboratory and the clinical microbiologist can play a pivotal role in any AMS program.
- Clinical laboratories can provide diagnostic stewardship, i.e., guidelines for appropriate specimen collection and information about when to reject inappropriate specimens.
- The microbiology laboratory should ensure that all antimicrobial susceptibility results are reported in a selective manner; ‘cascade reporting’ should be considered as part of an effective AMS program.
- Early and direct communication with the treating team regarding the interpretation of results and offering clinical advice can help support AMS initiatives and optimise antimicrobial therapy.
- Antibiograms can be used to help guide the local antimicrobial formulary, empiric antimicrobial guidelines and inform specific AMS interventions.
- WHONET is a software program available from the WHO to assist in the development of cumulative antibiograms.
The clinical microbiology laboratory
The clinical microbiology laboratory plays a pivotal role in any AMS program and can strengthen many implemented initiatives. The different components of an AMS program can be significantly enhanced by microbiology input.
The microbiology laboratory provides clinicians invaluable information that enables them to perform their daily duties and improve the quality of prescribing of antimicrobials. Laboratory information is often critical to clinical diagnoses and treatment decisions.
The clinical microbiologist has the potential to be involved in many aspect of the hospital's AMS program, including:
- membership of the drug and therapeutics committee (DTC);
- membership of the AMS committee;
- participation in the AMS team;
- education and resources to assist in AMS programs;
- development and review of clinical pathways and guidelines for the treatment of common infections; and
- preparation of antimicrobial susceptibility reports (antibiograms).
Diagnostic testing
The ability to correctly identify and diagnose infections will enable the rapid targeting of correct antimicrobial therapy or may even lead to the early cessation of therapy.
Rapid tests
Rapid diagnostic tests are increasingly being used to allow same-day analysis and identification, or within hours of growth. Using traditional approaches, it may take from 24 hours to 72 hours to identify the majority of cultured organisms. Therapeutic decisions about empiric choice of antimicrobials are, therefore, made while waiting for these culture results to be available. Due to the ever-increasing rates of multi-resistant organisms, in many settings broad-spectrum antimicrobials are being increasingly recommended for empiric therapy. Where available, these rapid tests do allow for the optimisation of antimicrobial choice in a timely manner, enabling a quicker transition from empiric to directed therapy.
Examples of rapid tests that may be available include:
- antigen/antibody detection tests;
- nucleic acid amplification tests;
- influenza from respiratory samples;
- methicillin-resistant Staphylococcus aureus from clinical specimens or infection control swabs;
- enteric pathogens from stool samples;
- susceptibility testing;
- semi-automated devices (e.g., Biomerieux Vitek, BD Phoenix, Beckman Coulter MicroScan);
- matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF); and
- peptide nucleic acid fluorescent in situ hybridisation (PNA FISH).
Implementation of rapid microbiological testing should be incorporated into AMS activities as appropriate. Without expert oversight of the interpretation of results, there is a risk that these tests will not be acted on in an appropriate or timely manner. With limited resources, choices around which tests should be implemented will require expert opinion on the cost-benefit equation of the introduction of new testing modalities, and will be guided by the local epidemiology, the complexity of running and interpreting the tests, the sensitivity and specificity of these tests, and the cost per specimen. A limitation of rapid testing is that these tests are still not able to effectively provide susceptibility information. This highlights the need for making accurate and up-to-date antibiogram information readily available to inform therapy choice. When rapid diagnostic tests are used in conjunction with AMS programs, they are able to improve patient care by decreasing the time to optimal therapy.
Antimicrobial serum level monitoring
The clinical microbiology laboratory, if able, should provide some monitoring of antimicrobial levels in the serum to aid clinicians to improve dosage of certain antimicrobials. This may occur in discussions with clinical chemistry and/or pharmacology units. At a minimum, this should occur for vancomycin and aminoglycosides. Other antimicrobials that may have serum levels monitored include antifungal agents, teicoplanin, and, in selected high-risk populations, β-lactams.
The results of any monitoring should be accompanied by expert comments to assist in the interpretation of these results and the requirement to improve prescribing dosage. Any monitoring of antimicrobial levels should be performed and reported in a timely manner in order to effect appropriate dosage changes and to avoid undertreatment or toxicity.
Procalcitonin
Procalcitonin is a prohormone of calcitonin that typically becomes elevated in bacterial infections but is rarely elevated in viral infections. It may be useful in helping to guide early cessation of empiric antibiotic therapy when the likelihood of bacterial infection is low. During treatment of bacterial infections, procalcitonin levels fall rapidly, which provides some objective measure of response to therapy. Some AMS programs have incorporated procalcitonin into their treatment guidelines to complement other methods of determining antimicrobial treatment duration.
The limitations of procalcitonin testing are that procalcitonin is also elevated in other inflammatory conditions (e.g., pancreatitis, major trauma and stress), and that its cost may be prohibitive for general use in some settings.
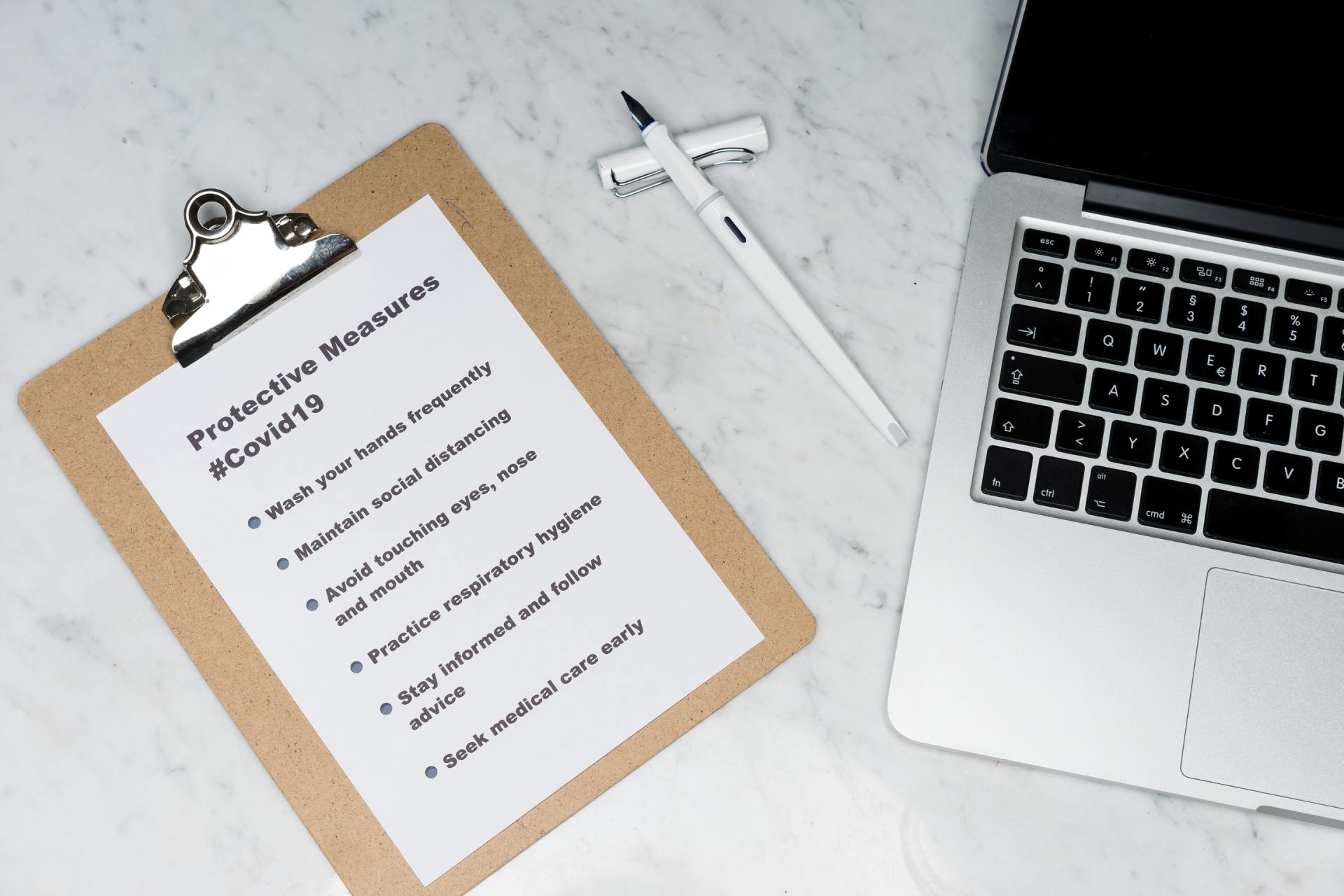
Diagnostic stewardship - specimen collection
Clinical laboratories can provide guidelines for appropriate specimen collection and information about when to reject inappropriate specimens. This is known as ‘diagnostic stewardship’. Diagnostic stewardship provides guidance and interventions to improve the use of microbiological diagnostics. This will in turn promote more appropriate and timely:
- collection of specimens;
- performance of diagnostic tests;
- selection of choice of cultured organisms to work-up, identify and report; and
- therapeutic decisions, leading to improved patient treatment.
An inappropriate specimen can lead to misleading information and negatively impact on the diagnostic decision-making process. The quality of the specimen should be commented upon, where possible, with some interpretation to help guide the prescriber.
Microbiology reporting
Microbiology reports should be accurate, concise, easy to understand and released in a timely manner to aid in the optimisation of antimicrobial therapy at the earliest possible time.
Comments to assist with the interpretation of findings are one of the most important ways that microbiologists can assist clinicians in choosing the appropriate therapy for their patients, in line with recommended guidelines.
Susceptibility results
Prescribing of antimicrobials to target isolated pathogens with specific resistance profiles is called ‘directed therapy’. Directed therapy using the narrowest-spectrum and effective antimicrobial agent typically improves patient outcomes, carries less risk of the development of AMR and is often the most cost-effective intervention. The time taken to effectively report information to the treating team will directly impact on the duration of empiric therapy and the time taken to switch to more effective directed therapy, or to the discontinuation of unnecessary antimicrobial treatment, including redundant dual therapy. Microbiology laboratories should have procedures in place to ensure the effective and timely communication of results, especially for critical isolates, which should be reviewed and updated regularly. This will in turn have an impact on improved patient outcomes, decreased lengths of hospital stay and improved overall health care costs.
Selective reporting
The microbiology laboratory should also ensure that antimicrobial susceptibility results are reported in a selective manner. Not all antimicrobial susceptibility results need to be released for every organism in every specimen. Selective reporting refers to the clinical microbiology laboratory’s critical appraisal of information on the choice of antimicrobials and bacterial susceptibilities that is to be released to the clinical team. The choice to suppress or release specific antimicrobial susceptibility results may be made for several reasons.
The microbiology laboratory should only report on those antimicrobials that are appropriate to the infection site. Not all antimicrobials are able to reach certain sites within the body at concentrations high enough to treat infections. For example, clindamycin would not be recommended for urinary tract infections and should not be reported on for isolates from urine specimens.
There should also be selectivity in the choice of antimicrobials for specific organisms. There are inherent resistance mechanisms that induce resistance within some bacteria when exposed to certain antimicrobials. For these antimicrobials, the susceptibilities should not be released. For example, you would not recommend ertapenem for Pseudomonas aeruginosa
and these susceptibility results will often be suppressed.
When reporting susceptibilities, aspects of the patient demographic data may also be considered. Such aspects as age, pregnancy status, etc., may be considered and the release of susceptibility results discouraged for antimicrobials that may not be appropriate for specific patient populations. For example, tetracyclines should not be used in children or during pregnancy.
There should also be a process for the work-up and reporting of contaminants, with commentary on the limited need for antimicrobial use. For example, for a sputum sample with few polymorphs and mixed upper respiratory flora on Gram stain, the report might contain a comment such as “the sample likely represents upper airway colonisation”. Similarly, a skin swab with few polymorphs and mixed skin flora might be reported as “mixed skin flora – likely colonisation”. For microbiological specimens that are deemed to be of insufficient quality, or those culturing only likely contaminants, the laboratory may decide to suppress these results pending further information. This might help to ensure that true infections are distinguished from contamination or colonisation, to help reduce the initiation of therapy when not indicated.
Typically, the microbiology laboratory should also only release results to agents listed as first-line in relevant evidence-based treatment guidelines. A second-line option for a person with an allergy to the first-line agent is often also provided. Reporting of restricted or non-formulary antimicrobials is usually avoided where possible.
Cascade reporting is a process of selective reporting whereby broader-spectrum antimicrobial susceptibility results are only released if the organism is resistant to the narrower-spectrum agents. Selective reporting with expert commentary on how to interpret the results has been shown to improve antimicrobial prescribing. There should always be a mechanism for the unreported susceptibility data to be readily available upon reasonable request. This may be added to the report: “further antimicrobial susceptibilities are available upon request – contact clinical microbiology to discuss further options”. Cascade reporting should be considered by all microbiology laboratories as part of an effective AMS program.
Clinician liaison
Early and direct communication with the treating team regarding the interpretation of results and clinical advice can help to support AMS initiatives and optimise antimicrobial therapy.
Critical results
For critical microbiology results (e.g., blood culture or cerebrospinal fluid positive results, or if a multi-resistant organism is identified), the results should ideally be urgently phoned though to the relevant treating physician to ensure that the appropriate treatment is not delayed.
Specialty units
Communication is especially important with specially groups, such as the intensive care unit or haematology/oncology units. This may consist of active ward-rounds within these units to discuss difficult patients and to offer expert advice and provide new results to the clinicians. As these specialty groups are often the highest users of antimicrobials and often have high rates of resistant organisms, there needs to be greater oversight of antimicrobial use to ensure appropriate use. This may be undertaken in conjunction with an infectious diseases physician, specialty pharmacist or nurse as part of an AMS round. This will also then have a flow-on effect in other units throughout the hospital as staff interact with these units and may help to control resistance within these high-risk units.
Antibiograms
Antibiograms are tables of antimicrobial susceptibility results grouped by pathogen that are collected over time. They may be used to help track changes in susceptibility over time, which might help to identify local outbreaks. They can be used to help guide local empiric antimicrobial guidelines. This may in turn influence the local antimicrobial formulary and inform specific AMS interventions.
Antibiograms might be utilised by national bodies to inform national guidelines. Antibiograms should ideally be produced on at least an annual basis by the clinical microbiology laboratory. At a minimum, they should be produced for common local or high-risk pathogens, (e.g., Escherichia coli
or Staphylococcus aureus), important clinical conditions (e.g., bacteraemia and urinary tract infection) or for patients in specific high-risk locations, (e.g. the intensive care unit).
As the DTC, AMS team and specialty groups will utilise the antibiograms to inform guidelines and treatment pathways, it is important to communicate how these data were developed and which patient populations and circumstances they apply to. In resource-poor settings where only the sickest patients, or those who have failed empiric therapy, may have specimens taken, the antibiogram susceptibility data may be biased towards groups that may be at a higher risk of colonisation with multi-resistant organisms. Consequently, the antibiogram may not be entirely relevant in guiding the empiric choice of therapy selected for the general inpatient group. When the threshold for testing is high (e.g., due to cost constraints), the specimens contributing to the antibiogram may only reflect heavily pre-treated or the most severely ill patients. These should, therefore, not be used to infer the likely susceptibility patterns of isolates from all patients.
A clinical microbiologist is required to assist in the interpretation of these results and antibiograms should be reported to the clinicians or groups responsible for advising on local prescribing guidelines, including, the AMS team, DTC, quality committees, infectious diseases department, intensive care unit, etc. If there is no access to clinical microbiological expertise, it may be required that the AMS team obtain data from external laboratories and develop their own antibiograms.
There are resources available to assist in the preparation of these:
WHONET
is a software program available from the WHO that can assist in the development of cumulative antibiograms. It can upload data from pathology information systems providing the information base required to produce an institutional antibiogram.
For small hospitals it may be difficult to produce useful antibiograms as it is suggested that at least 30 isolates of each organism are required. It may, therefore, be more beneficial to produce regional antibiograms by combining data from hospitals with similar population characteristics.
The role of microbiologists in education
Education on the following can be undertaken:
- aseptic technique;
- correct techniques for microbiological specimen collection and transport;
- when and which microbiology specimens should be collected and interpretation of these results;
- infection versus colonisation or contamination; and
- interpretation of antibiograms for relevant staff.
Improving diagnostic accuracy can have a major impact on the appropriateness of antimicrobial prescribing. Providing some guidance during the pre-analytic phase of microbiology specimen collection can improve the quality of the specimen, ensuring more accurate and diagnostically significant results are attained. Procedures for when to reject inappropriate specimens or limit the work-up of suspected contaminants or colonisers are likely to decrease the use of antimicrobials. This will impact on the choice of antimicrobials selected and give clinicians greater confidence in de-escalating or ceasing unnecessary therapy. Laboratory guidelines, policies and procedures that ensure high-quality specimen collection, transport and processing have a key role in reducing inappropriate antimicrobial use, by ensuring the clinical applicability of the microbiology results.
Clinical microbiology laboratories are key to AMS programs, providing specimen collection and testing, rapid diagnostics, susceptibility testing, and production of antibiograms and education activities.