Hospitals
Tertiary hospitals stream
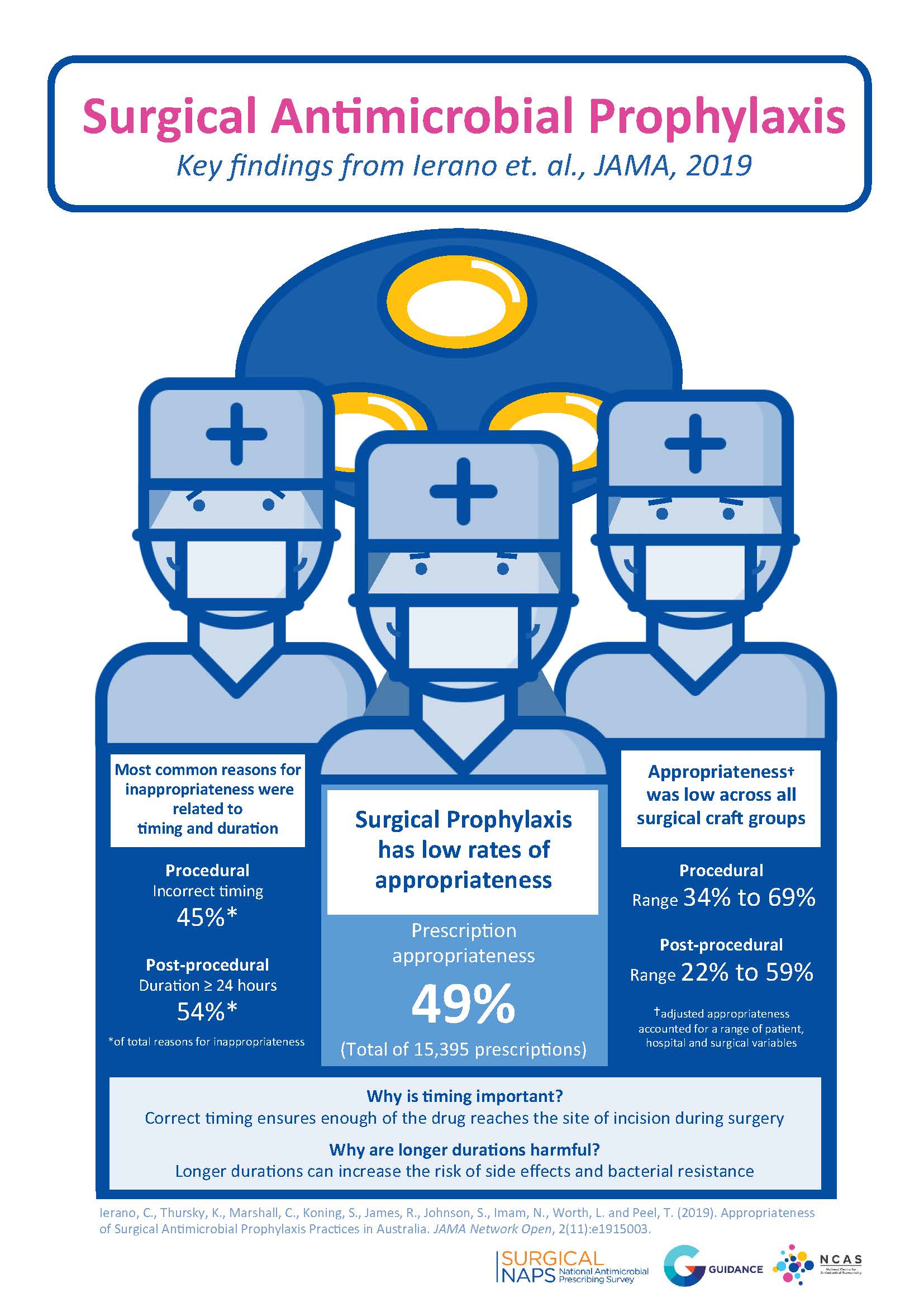
Surgical antimicrobial prophylaxis (SAP) was identified as the most common indication or reason for antibiotics in tertiary hospitals in Australia during the National Antimicrobial Prescribing Survey
(NAPS) that was performed in November 2013 and in subsequent NAPS audits. SAP is an important strategy for the prevention of surgical site infections; however, in the 2013 NAPS survey, ~50% of surgical antibiotic prophylaxis use was inappropriate, particularly because of prolonged duration or inappropriate agent selection. NCAS developed the Surgical NAPS audit tool to specifically focus on SAP prescribing and to assist hospitals to more closely monitor and improve their SAP prescribing.
The aims of our research on SAP prescribing are to:
• Develop a framework for antimicrobial stewardship (AMS) interventions for SAP prescribing.
Antifungal infections, particularly in the immunocompromised and immunosuppressed setting, can be difficult to manage. Increases in rates of antifungal resistance are concerning, as such increases further jeopardise outcomes and the safety and quality of care for high-risk patients, including cancer and transplant patients. Currently, there is insufficient data on the prevalence and quality of antifungal use in Australian hospitals, and strategies for antifungal stewardship (AFS).
The aims of our research on antifungal use and AFS are to:
• Describe current AFS strategies in place and how antifungal use is monitored in Australian hospitals;
• Describe the key AFS metrics that measure the impact of AFS programs on antifungal prescribing and patient outcomes;
• Describe factors that influence posaconazole plasma concentrations and the utility of therapeutic drug monitoring for posaconazole prophylaxis with the oral tablet formulation;
• Describe current antifungal prescribing practices in Australian liver transplant units;
• Design and develop antifungal use surveillance programs; and
• Design and develop AFS strategies for Australian hospitals.
While some hospitals in Australia have well-established hospital-in-the-home (HITH) services, where patients are provided care in their own homes, there is insufficient information on the prevalence and quality of antimicrobial use in HITH services. As many HITH services provide antimicrobial therapy at home, it is important to investigate the quality of antimicrobial use in HITH services and explore opportunities for AMS.
The aim of our research on antimicrobial use and AMS in the HITH setting is to:
• Analyse the prevalence and quality of antimicrobial prescribing in HITH services in Australia, and provide this data to HITH services.
Regional & remote hospitals stream
Regional and remote hospitals face major challenges with developing and implementing AMS because of differences in patient mix, workforce and existing service delivery structures. AMS in smaller Australian hospitals is in its infancy. The institutions rely on affiliations with larger metropolitan hospitals for antimicrobial prescribing advice.
NCAS researchers will test models for AMS in regional and remote hospitals. The models will be adapted to suit the sites but it is intended that telehealth links to a tertiary hospital will be used to provide regular contact for individualised post-prescription review, in addition to a computerised approval system for nominated restricted medicines, structured education, and regular audit and feedback. New modules of Guidance, an AMS workflow tool developed by Melbourne Health, have been developed to further improve documentation and communication of advice, and these are likely to assist in telehealth consultations.
At the conclusion of the projects proposed, we will have identified and tested interventions to improve antimicrobial prescribing that are feasible and translatable from large hospitals to rural and regional sites with limited resources.
The aims of our research on regional and remote hospitals are to:
• Design and implement a cellulitis bundle of care in a collaborative project involving multiple regional hospitals in Victoria.
In many regional (and some metropolitan) hospitals, nurses may have responsibility for quality of medicine use processes and programs. While nurses' contribution to augmenting the safety and quality of patient care is well-recognised, their role in AMS is less well-understood.
The aims of our research on the role of nurses in AMS in Australia are to:
• Describe international models involving nurses in AMS;
• Describe the views and preferences of Australian nurses regarding AMS;
• Describe the perceived learning needs of nurses in relation to AMS and how these can be addressed;
• Assess how nurses can play a leadership role in AMS programs; and
• Design and implement an educational intervention targeting specific AMS strategies to increase nurses’ knowledge, confidence and use of skills in practice.